A . Purpose of the Action
HHS/CDC has statutory authority (42 U.S.C. 264, 265) to promulgate regulations which protect U.S. public health from communicable diseases, including quarantinable communicable diseases as specified in Executive Order of the President. See Executive Order 13295 (April 4, 2003), as amended by Executive Order 13375 (April 1, 2005) andExecutive Order 13674 (July 31, 2014). The need for this proposed rulemaking was reinforced during HHS/CDC’s response to the largest outbreak of Ebola virus disease (Ebola) on record, followed by the recent outbreak of Middle East Respiratory Syndrome (MERS) in South Korea, both quarantinable communicable diseases, and repeated outbreaks and responses to measles, a non-quarantinable communicable disease of public health concern, in the United States. The provisions contained within this proposal will enhance HHS/CDC’s ability to prevent the further importation and spread of communicable diseases into the United States and interstate by clarifying and providing greater transparency regarding its response capabilities and practices.
B. Summary of Major Provisions
Both the domestic and foreign portions of this NPRM include new proposed public health definitions; new proposed regulatory language codifying HHS/CDC’s activities concerning implementation of non-invasive public health prevention measures (i.e., traveler health screening) at U.S. ports and other U.S. locations (i.e., railway stations, bus terminals); and proposed provisions for affording persons served with a Federal public health order (e.g., isolation, quarantine) with due process, including requiring that HHS/CDC explain the reasons for issuing the order, administrative processes for appealing the order, and a mandatory reassessment of the order.
In addition, the domestic portion of this NPRM also proposes reporting requirements for commercial passenger flights of death or illness to CDC; a provision allowing for implementation of travel restrictions and issuance of travel permits by CDC for individuals under Federal quarantine, isolation, or conditional release orders, or in response to a state or local request for assistance; and new regulatory language clarifying when an individual who is moving between U.S. states is “reasonably believed to be infected” with a quarantinable communicable disease in a “qualifying stage,” which determines whether such an individual may be apprehended or examined for potential infection with a quarantinable communicable disease. The foreign portion of this NPRM also proposes new regulatory authority permitting the CDC Director to prohibit the importation of animals or products that pose a threat to public health. HHS/CDC is also proposing to change the text of the current regulation to reflect modern terminology, technology, and plain language currently used by private industry, public health partners, and the public. The NPRM further authorizes expanded forms of public health monitoring, beyond an in-person visit by a public health officer, for individuals who are reasonably believed to be exposed to or infected with a quarantinable communicable disease and subject to a conditional release order. This would include monitoring through electronic and internet-based means, such as email and webcam application tools. Finally, while neither modifying nor authorizing additional criminal penalties for violations of quarantine rules and regulations, this NPRM updates regulatory language to align with existing criminal penalties set forth in statute.
C. Summary of Costs and Benefits
The regulatory impact analysis quantitatively addresses the costs and benefits associated with this NPRM. The economic impact analysis of this NPRM is subdivided into four sections.
The first analysis is of proposed 42 CFR 70.1, 42 CFR 71.1/71.4/71.5 for which the primary costs for submitting passenger and crew information to HHS/CDC are incurred by airlines and vessel operators and the primary benefit is improved public health responsiveness to assess and provide post-exposure prophylaxis to travelers potentially exposed to communicable diseases of public health concern. The most likely estimates of annual costs to airlines, vessel operators, the United States government, and public health departments are low ($35,785, range $10,959 to $65,644) because the NPRM primarily codifies existing practice or improves alignment between existing regulatory text as well as the International Civil Aviation Organization (ICAO)’s guidelines for symptoms to report. The cost estimates in this NPRM are based on an anticipated small increase in the number of illness reports delivered by airlines and processed by HHS/CDC and increased costs for airlines and vessel operators to comply with HHS/CDC orders for traveler and crew contact data, to the extent that such information is readily available and already maintained. The cost estimate also includes an increase in costs for public health departments to contact more exposed travelers due to the availability of improved contact data.
The best estimate of the annual quantified benefits of the NPRM are $117,376 (range $26,337 to $312,054) and mostly result from increased efficiencies for HHS/CDC and state and local public health departments to conduct contact investigations among travelers on an aircraft exposed to communicable diseases of public health concern, especially for measles and tuberculosis. To the extent that improved responsiveness of airlines to HHS/CDC traveler data orders may result from the implementation of the provisions proposed in this NPRM, HHS/CDC may become better able to respond to infectious diseases threats and (1) reduce case-loads during infectious disease outbreaks, (2) reduce public anxiety during disease outbreaks, (3) mitigate economic impacts on businesses as a consequence of reduced public anxiety, and (4) reduce the amount of personnel labor time to conduct large-scale contact investigations in response to a new infectious disease or one with larger scale public health and medical consequences like Ebola.
The second analysis in this NPRM is of a number of provisions that aim to improve transparency of how HHS/CDC uses its regulatory authorities to protect public health. These changes are not intended to provide HHS/CDC with new regulatory authorities, but rather to clarify the agency’s standard operating procedures and policies with regard to existing regulations in 42 CFR parts 70 and 71 including due process rights for individuals. HHS/CDC believes that such clarity is an important qualitative benefit of the provisions proposed in this NPRM, but it is not able to monetize this increase in clarity in a robust way. Although the provisions updated in this NPRM do not provide HHS/CDC with new regulatory authority, the 2014-16 Ebola Entry Risk Assessment program is used the demonstrate the economic impact of the implementation of activities associated with these authorities.
The third analysis is of the proposed revisions to 42 CFR 70.13/71.30: Payment for Care and Treatment, which are not expected to lead to a change in HHS/CDC policy under which HHS/CDC may act as the payer of last resort for individuals subject to medical examination, quarantine, isolation, and conditional release under Federal orders. The primary benefit of codification is increased transparency around HHS/CDC policies to assist in paying for treatment for individuals under Federal orders. The analysis for these provisions is an examination in potential transfer payments between HHS/CDC and healthcare facilities that provide treatment to individuals under Federal orders. Because this analysis deals only with transfer payments between HHS/CDC, any marginal costs to HHS/CDC associated with a change in payments would correspond exactly to a benefit to healthcare facilities. In the absence of the NPRM, the only possible change to the current baseline is an unanticipated precedent-changing event, which would require an increase in payments from HHS/CDC to healthcare treatment facilities. The resulting extreme upper bound estimate of the provisions in the NPRM would be a benefit of $500,000 to HHS/CDC and a corresponding cost to healthcare facilities of $500,000.
The fourth analysis is of the impact of the proposed 42 CFR 71.63: Suspension of entry of animals, articles, or things from designated foreign countries and places into the United States. In this NPRM, HHS/CDC is elucidating its authority to temporarily suspend entry of animals, articles or things from designated foreign countries and places into the United States. HHS/CDC cannot predict how often such authority may be used in the future or for what animal, article or thing. HHS/CDC previously exercised this authority on June 11, 2003, “when under 42 CFR 71.32(b), HHS/CDC implemented an immediate embargo on the importation of all rodents from Africa (order Rodentia).” This embargo was necessary to halt transmission of a monkeypox outbreak in the United States, which caused 71 cases (16 hospitalized). Most cases resulted from contact with prairie dogs after monkeypox had been transmitted from African rodents to prairie dogs as part of the U.S. pet trade.
A simple economic impact analysis of this embargo is performed to demonstrate the costs and benefits of such actions, but HHS/CDC does not anticipate an increase in frequency of such actions based on the provisions included in this NPRM. The primary purpose of the analysis is to demonstrate potential costs and benefits using a realistic example. Based on this simple analysis, the annual cost associated with the embargo of African rodents is estimated to be around $19,000. An average of 959 rodents per year were imported in the three years preceding the embargo (2000-2002). In comparison a very conservative estimate of some of the cost of the monkeypox outbreak is $3.3 million inclusive of illness costs to persons contracting monkeypox in the United States, a portion of HHS/CDC and local and state health department monkeypox outbreak response costs, and a one-time cost to the U.S. domestic prairie dog market. Comparing the benefits associated with the avoidance of a re-introduction of the monkeypox virus to the United States with the annual costs to the African rodent import market, the benefits of the embargo are likely to greatly exceed the cost. The permanent restriction of African rodent imports to the United States was later codified in current 42 CFR 71.56.
II. Public ParticipationBack to Top
Interested persons or organizations are invited to participate in this rulemaking by submitting written views, recommendations, and data on all aspects of the proposed rule. Comments received should reference a specific portion of the rule, and inclusion of any attachments and other supporting materials, are part of the public record and subject to public disclosure. Do not include any information in your comment or supporting materials that you consider confidential or inappropriate for public disclosure. HHS/CDC will carefully consider and address all comments submitted and may revise the content of the rule as appropriate at the final rulemaking stage. HHS/CDC will publish a final rule after the comment period that reflects any content changes made as a result of comments received. As emphasized in the text below, HHS/CDC would appreciate public comment on data collection and any privacy concerns associated with this process, public health prevention measures, contact tracing, medical review process, and the availability of assistance for individuals who are indigent.
III. BackgroundBack to Top
A. Legal Authority
The primary legal authority supporting this rulemaking is sections 361 and 362 of the Public Health Service Act (42 U.S.C. 264, 265). Section 361, among other things, authorizes the Secretary [1] of HHS to make and enforce such regulations as in the Secretary’s judgment are necessary to prevent the introduction, transmission, or spread of communicable diseases from foreign countries into the states or possessions of the United States and from one state or possession into any other state or possession. Such regulations currently define communicable disease as an illness due to a specific infectious agent or its toxic products which arises through transmission of that agent or its products from an infected person or animal or a reservoir to a susceptible host, either directly or indirectly through an intermediate animal host, vector, or the inanimate environment. See 42 CFR 70.1, 71.1. Such regulations also define possession as a U.S. territory meaning any territory of the United States, including American Samoa, Guam, the Northern Mariana Islands, the Commonwealth of Puerto Rico, and the U.S. Virgin Islands. See 42 CFR 70.1, 71.1. On August 16, 2000, the Secretary transferred the authority for interstate control of communicable disease, including the authority to apprehend, examine, detain, and conditionally release individuals moving from one state into another from the U.S. Food and Drug Administration (FDA) to CDC. This authority is implemented in 42 CFR part 70. FDA retained its concurrent regulatory authority under section 361 of the Public Health Service Act for purposes of regulating animals and other products that may transmit or spread communicable diseases interstate. Thus, both CDC and FDA may take actions under section 361 of the Public Health Service Act to prevent interstate spread of communicable diseases in regard to animals or products, though in practice such actions would be coordinated internally between these agencies. The Secretary took this action to consolidate regulations designed to control the spread of communicable diseases, thereby increasing the efficiency and effectiveness of both agencies. This rule is not intended to have any effect upon FDA’s authority under section 361 of the Public Health Service Act. Authority for carrying out CDC’s functions under sections 361-369 (42 U.S.C. 264-272) has been delegated to HHS/CDC’s Division of Global Migration and Quarantine (DGMQ). Regulations that implement Federal quarantine authority are currently promulgated in42 CFR parts 70 and 71. Part 71 contains regulations to prevent the introduction, transmission, and spread of communicable diseases into the states and territories of the United States, while part 70 contains regulations to prevent the introduction, transmission, or spread of communicable diseases from one state or U.S. territory into another.
Section 361 (42 U.S.C. 264) is divided into five subsections, (a)-(e). Section 361(a) (42 U.S.C. 264(a) states that the Secretary may make and enforce regulations as necessary to prevent the introduction, transmission, and spread of “communicable diseases” from foreign countries into the United States or from one state or possession (U.S. territory) into any other state or possession (U.S. territory). By its terms, subsection (a) does not seek to limit the types of communicable diseases for which regulations may be enacted, but rather applies to all communicable diseases that may impact human health. Section 361(a) (42 U.S.C. 264(a)) further authorizes the Secretary to promulgate and enforce a variety of public health regulations to prevent the spread of these communicable diseases including: Inspection, fumigation, disinfection, sanitation, pest extermination, destruction of animals or articles found to be sources of dangerous infection to human beings, and other measures. In contrast, section 361(b) (42 U.S.C. 264(b)) authorizes the “apprehension, detention, or conditional release” of individuals for the purpose of preventing the introduction, transmission, and spread of a limited subset of communicable diseases, specifically those communicable diseases specified in an Executive Order of the President, upon recommendation of the Secretary in consultation with the Surgeon General. HHS/CDC refers to this limited subset of communicable diseases as “quarantinable communicable diseases” because these are the communicable disease for which by statute quarantine, isolation, or conditional release are authorized. Section 361(c) (42 U.S.C. 264(c)) states that, except as provided in subsection (d), regulations regarding apprehension, detention, examination, or conditional release shall only be applicable to individuals coming into a state or U.S. territory from a foreign country or U.S. territory. 42 U.S.C. 264(c). Thus, subsection (c) provides the basis for the quarantine, isolation, or conditional release of individuals arriving into the United States from foreign countries for the purposes of preventing the introduction, transmission, and spread of quarantinable communicable diseases (as specified by Executive Order) while subsection (d) provides the statutory basis for interstate quarantine, isolation, and conditional release measures.
Section 361(d)(2) (42 U.S.C. 264(d)(2)) imposes two main requirements on the interstate quarantine, isolation, or conditional release of individuals: (1) The qualifying-stage requirement; and (2) the requirement for an effect on interstate movement. Both of these requirements must be satisfied. Subsection (d) states that regulations may provide for the apprehension and examination of any individual “reasonably believed to be infected with a communicable disease in a qualifying stage.” 42 U.S.C. 264(d)(1). As defined by this subsection, a “qualifying stage” means that the communicable disease is in “a precommunicable stage, if the disease would be likely to cause a public health emergency if transmitted to other individuals” or “a communicable stage.” 42 U.S.C. 264(d)(2). The subsection further states that if upon examination any such individual is found to be infected, he or she may be detained for such time and in such manner as may be reasonably necessary. 42 U.S.C. 264(d)(1). In addition to the qualifying-stage requirement, this subsection further requires a reasonable belief that the individual: (A) Be moving or about to move from a state to another state; or (B) be a probable source of infection to individuals who, while infected with such disease in a qualifying stage, will be moving from a state to another state. 42 U.S.C. 264(d)(1).
As provided for under section 361(b) (42 U.S.C. 264(b)), the Secretary’s authority to allow for the apprehension, examination, detention, and conditional release of individuals is limited to those communicable diseases specified in an Executive Order of the President, i.e.,“quarantinable communicable diseases.” These quarantinable communicable diseases currently include cholera, diphtheria, infectious tuberculosis (TB), plague, smallpox, yellow fever, and viral hemorrhagic fevers (such as Marburg, Ebola, Lassa fever, and Crimean-Congo), severe acute respiratory syndromes,2 and influenza caused by novel or re-emergent influenza viruses that are causing or have the potential to cause a pandemic. Executive Order 13295 (April 4, 2003), as amended by Executive Order 13375 (April 1, 2005) andExecutive Order 13674 (July 31, 2014).
Lastly, section 361(e) (42 U.S.C. 264(e) states that nothing in this section nor in section 363 (42 U.S.C. 266) (a different section authorizing quarantine in time of war) nor in regulations promulgated under these sections, shall be construed as superseding any provision under state law (including in regulations and provisions established by political subdivisions of states), except to the extent that such provisions conflict with the exercise of Federal authority. Accordingly, by its plain language, section 361 (42 U.S.C. 264) does not preempt state or local public health laws or regulations, except in the event of a conflict with the exercise of Federal public health authority.
In addition to section 361 (42 U.S.C. 264), HHS/CDC believes that the following Public Health Service Act sections are also relevant with respect to this rulemaking: Section 311 (42 U.S.C. 243), section 321 (42 U.S.C. 248), section 322 (42 U.S.C. 249), section 362 (42 U.S.C. 265), section 365 (42 U.S.C. 268), and sections 367-69 (42 U.S.C. 270-72). Section 311 authorizes the Secretary to accept state and local assistance in the enforcement of quarantine rules and regulations and to assist states and their political subdivisions in the control of communicable diseases. Section 321 provides for the selection, establishment, control, management, and operation of institutions, hospitals, and stations as may be necessary to carry out public health functions. Section 322 authorizes payment for the care and treatment, in a public or private facility, of individuals detained in accordance with quarantine laws. Section 362 authorizes (in accordance with regulations approved by the President 3 ) suspending the entry of imports into the United States based on the presence of a communicable disease in a foreign country or place. Section 365 provides that it shall be the duty of customs officers (e.g., U.S. Customs and Border Protection officers) and of U.S. Coast Guard officers to aid in the enforcement of quarantine rules and regulations. Section 367 authorizes the application of certain sections of the Public Health Service Act and promulgated regulations (including penalties and forfeitures for violations of such sections and regulations) to air navigation and aircraft to such extent and upon such conditions as deemed necessary for safeguarding public health.
As prescribed in section 368 (42 U.S.C. 271) and under 18 U.S.C. 3559 and 3571(c), criminal sanctions exist for violating regulations enacted under sections 361 and 362 (42 U.S.C. 264 and 265). 18 U.S.C. 3559 defines an offense (not otherwise classified by letter grade) as a “Class A misdemeanor” if the maximum term of imprisonment is “one year or less but more than six months.” 18 U.S.C. 3571 provides that individuals found guilty of an offense may be sentenced to a fine. Specifically, an individual may be fined “not more than the greatest of”—(1) the amount specified in the law setting forth the offense; or (2) for a misdemeanor resulting in death, not more than $250,000; or (3) for a Class A misdemeanor that does not result in death, not more than $100,000. Similarly, an organization, found guilty of an offense may be fined “not more than the greatest of”—(1) the amount specified in the law setting forth the offense; or (2) for a misdemeanor resulting in a death, not more than $500,000; or (3) for a Class A misdemeanor that does not result in death, not more than $200,000. 42 U.S.C. 271 sets forth statutory penalties of up to 1 year in jail and a fine of $1,000. Therefore, it is classified as a Class A misdemeanor under 18 U.S.C. 3559. Because the alternate fines set forth under 18 U.S.C. 3571 are greater than the $1,000 set forth under 42 U.S.C. 271 (which sets a maximum penalty of not more than $1,000 or one year of jail, or both for violation of quarantine laws), and because 42 U.S.C. 271 does not exempt its lower penalties from 18 U.S.C. 3571(e), HHS/CDC plans to codify the greater penalties of 18 U.S.C. 3571(b)(5) and (c)(5) and to remove the lower penalties as stated in 42 CFR 71.2 from the regulation.
Lastly, section 369 (42 U.S.C. 272) provides that quarantine officers are authorized to take declarations and administer oaths in matters pertaining to the administration of quarantine laws and regulations of the United States.
B. Historical Background for This Rulemaking
On November 30, 2005, HHS/CDC published a notice of proposed rulemaking (70 FR 71892) proposing to update its existing foreign and interstate quarantine regulations to prevent the introduction, transmission, or spread of communicable diseases from foreign countries into the U.S. and from one State or U.S. territory into another. HHS/CDC received extensive comments on this proposed rulemaking. The 2005 proposed rule would have required airlines and vessels to request certain information from passengers and crew and to maintain data in an electronic database for 60 days following the culmination of the flight or voyage. The proposed rule would have also modified Federal regulations governing the apprehension, detention, examination, and conditional release of individuals reasonably believed to be infected with a quarantinable communicable disease. CDC received significant comment on the 2005 NPRM from industry that felt that the development of the passenger information data storage system was overly burdensome.
HHS/CDC also received comments contending that its procedures for quarantine and isolation lacked clarity and, in some instances, were not sufficiently protective of the individual. For instance, the 2005 proposal used the term “provisional quarantine” to denote the time period during which an individual could be held pending the issuance of a written order for quarantine, isolation, or conditional release or confirmation that the individual was not infected with a quarantinable communicable disease. The 2005 proposal also stated that “provisional quarantine” could last up to 3 business days. CDC received public comments that the term “provisional quarantine” was inconsistent with public health practice and that relying on “business days” which by definition excludes weekends and holidays was inappropriate. In response, the current proposal does not use the term “provisional quarantine,” but rather uses the term “apprehension” which is a statutory term used in section 361 of the Public Health Service Act (42 U.S.C. 264(c) and (d)(1)), and is defined in this proposal as “the temporary taking into custody of an individual or group for purposes of determining whether Federal quarantine, isolation, or conditional release is warranted.” Furthermore, as explained in the preamble text explaining the use of the term “apprehension,” based on past experience, HHS/CDC believes that the service of a written order for quarantine, isolation, or conditional release can generally be accomplished within 24-48 hours of an apprehension. Moreover, while the 2005 proposal stated that individuals subject to an order for quarantine, isolation, or conditional release could “authorize a representative” for purposes of a medical review hearing, the proposal did not have any provision authorizing Federal appointment of such a representative for individuals who are indigent. Accordingly, in response to public comments criticizing the lack of such an appointment, the current proposal contains specific language authorizing the appointment of a “medical representative” for anyone who qualifies as “indigent.” Proposed definitions for “medical representative” and “indigent” are contained in this current proposal and HHS/CDC invites public comment on these proposed definitions as well as the proposed “apprehension” activities.
HHS/CDC ultimately did not publish a final rule based on this 2005 proposal and since that time its views have been informed by the public health response to more recent communicable disease outbreaks, including Ebola, MERS, and continuing sporadic outbreaks of measles. Through the publication of today’s NPRM, CDC is formally withdrawing the 2005 NPRM and submitting a new proposal for public comment. Notably, today’s proposal does have some similarities with the 2005 proposal, for instance by proposing specific provisions governing the content of written Federal orders for quarantine, isolation, and conditional release, proposed procedures for administrative hearings to review these written Federal orders, and a specific provision governing the content and compiling of an administrative record. However, today’s proposal is more limited in scope than the 2005 proposal and does not contain any provisions affecting Tribal lands, authorizing quarantine “in time of war,” or altering HHS/CDC practices in regard to “bills of health” or yellow fever vaccination centers.
On December 26, 2012, HHS/CDC simultaneously published two direct final rules (DFR) and notices of proposed rulemaking (NPRM) to update the Scope and Definitions in both parts 70 (77 FR 75880 and 77 FR 75936) and 71 (77 FR 75885 and 77 FR 75939) to reflect modern terminology and plain language used globally by industry and public health partners. HHS/CDC did not receive significant adverse comment to either proposals and on February 25, 2013, published notices in the Federal Register confirming the effective dates of the DFRs (February 25, 2013) (78 FR 12621 and 78 FR 12622) and withdrawing the NPRMs from rulemaking (78 FR 12702).
IV. Rationale for Notice of Proposed RulemakingBack to Top
A timely and efficient public health response during an outbreak is critical to preventing the introduction, transmission or spread of communicable disease. Globally, there are several current and recurring communicable disease outbreaks imminently threatening human health and safety. Ebola, also known as Ebola hemorrhagic fever or Ebola virus disease, is a rare and deadly disease caused by infection with one of the Ebola virus strains. The 2014-2016 Ebola epidemic was unprecedented in its scope and complexity, and it triggered the largest public health response in CDC’s history. Outbreaks begin when Ebola is transmitted from an infected animal to a human, and then from human to human. Animal species carrying viruses that are capable of infecting humans are known as reservoir hosts.4 For Ebola, fruit bats are believed to be the reservoir. 5 6However, it is unclear whether the first infected human in the outbreak was infected with Ebola directly from a bat, or whether a second, intermediate animal host, such as a nonhuman primate (e.g., monkeys, gorillas, and chimpanzees) or duiker (a type of forest antelope), was involved. 7 8 The virus can be transmitted from animal to human via contact with bodily fluids of infected animals. In West Africa, it’s not uncommon for people to come into contact with animals while hunting or preparing food. As of the date of publication of this NPRM, although progress has been made and vaccine trials are underway in West Africa, there is no approved vaccine for Ebola, nor is there specific approved antiviral treatment.
As of March 3, 2016, a total of 28,603 cases of Ebola and 11,301 deaths have been reported worldwide. 9 10 The majority of cases occurred in Guinea, Liberia and Sierra Leone, with smaller outbreaks in Nigeria and Mali, and cases exported to four other countries including the United States. Liberia was first declared free of Ebola virus transmission (as defined by zero cases for at least 42 days) by the World Health Organization (WHO) on May 9, 2015; Sierra Leone on November 7, 2015; and Guinea on December 29, 2015. On January 14, 2016, WHO officially declared all three countries that were hardest-hit (Guinea, Liberia, and Sierra Leone) to be free of Ebola virus transmission for the first time since the start of the epidemic more than two years ago. However, each of the three countries has experienced one or more clusters of Ebola cases after having initially been declared free of Ebola transmission, and WHO warns that new cases could still appear because the virus can be transmitted through sexual activity with some male Ebola survivors for as long as one year after infection, and that efforts are still needed to prevent and respond to any new outbreaks. [11]
Before the 2014-2016 Ebola epidemic in West Africa, reports of Ebola exportation to other countries were rare, a fact generally attributed in part to the remote, rural locations of previous outbreaks. The establishment of Ebola transmission in 2014 in the capital cities of Guinea, Liberia and Sierra Leone, with large populations and international airports and other connections to international transportation networks, raised concerns about the potential for spread through international travel to other parts of the world. These concerns were validated by the recognition of at least eight exported cases, three of which resulted in additional spread and infection of 29 people. [12]
In October, 2014, after a case of Ebola was imported and identified in the United States from West Africa, resulting in two domestic cases and extensive contact investigations of travelers onboard aircraft and the larger community, questions were raised concerning whether HHS/CDC should strengthen the domestic response to Ebola by prohibiting travel to the United States from the three countries with widespread transmission. HHS/CDC projected that such a travel ban would cause greater harm than good to the public health response by hampering travel of responders and delivery of supplies into the region, and could paradoxically increase the risk of spread via potentially infected individuals engaging in travel through covert and circuitous travel routes. Instead, HHS/CDC recommended that public health authorities assume the responsibility for monitoring of all travelers arriving from countries with Ebola outbreaks. Because complete and timely contact information was not available for these travelers, in-person questioning at the arrival airport was required to gather such information.
Therefore, in response to the imported Ebola case, as well as consideration of potential response activities, beginning October 11, 2014, HHS/CDC and the U.S. Department of Homeland Security (DHS) began a new enhanced entry risk assessment and management program at the five U.S. international airports that routinely received approximately 90 percent of travelers from Guinea, Liberia, and Sierra Leone: New York’s John F. Kennedy, Washington-Dulles, Newark Liberty, Chicago-O’Hare, and Atlanta Hartsfield Jackson. [13] This operation of unprecedented magnitude required coordination of multiple U.S. Government agencies, as well as airport authorities and health departments in all U.S. states and territories. Travelers from Mali were later added on November 17, 2014, in response to an outbreak in that country; Mali’s outbreak was short-lived, and enhanced entry risk assessment and management for travelers from Mali was discontinued on January 6, 2015. Following the declaration that the outbreak had ended in Liberia and the establishment of control measures in that country, on September 21, 2015, the United States discontinued enhanced entry risk assessment and management for travelers from Liberia. On November 7, 2015, WHO declared Sierra Leone free of Ebola virus transmission and enhanced entry risk assessment and management for travelers from Sierra Leone was discontinued on December 22, 2015. In addition, Guinea was declared free of Ebola virus transmission on December 29, 2015, and enhanced entry risk assessment and management for travelers from Guinea was discontinued on February, 19, 2016, thus bringing an end to the enhanced entry risk assessment and management program in the US. Between October 11, 2014 and February 19, 2016, enhanced entry risk assessment was conducted for approximately 38,000 travelers.
A second relevant example of the importance of CDC improving the efficiency of it public health response is illustrated by CDC’s response to two imported cases of MERS into the United States in 2014. While no additional transmissions occurred as a result of these importations, the subsequent investigation required the tracking and monitoring of more than 700 household, healthcare, community, and travel-related contacts, including almost 650 travelers onboard commercial aircraft. If the cost estimates in the RIA for the average cost per contact to CDC ($180) and to public health departments ($180) [14] are applied to these investigations (704 contacts), the total cost to evaluate MERS contacts would be approximately $250,000. However, this may underestimate the actual cost if state and local health departments deployed more resources per contact to locate MERS contacts more rapidly than would be the case for contact investigations for diseases more commonly reported in the United States (e.g., tuberculosis). First identified and reported to cause severe acute respiratory infection in September 2012, MERS has caused infections worldwide, with at least 25 countries reporting cases to date. All reported cases have been directly or indirectly linked through travel or residence to nine countries: The Kingdom of Saudi Arabia (KSA), the United Arab Emirates (UAE), Qatar, Jordan, Oman, Kuwait, Yemen, Lebanon, and Iran. The majority of cases (~85%) have been reported from KSA, where there is strong evidence for ongoing, sporadic introductions from animals (e.g., camels) to humans, followed by both healthcare-related and community human-to-human transmission. In May 2015, a case in a person who had travelled through several countries in the Arabian Peninsula and returned to the Republic of Korea started the largest outbreak of MERS outside of the Arabian Peninsula. The Korea outbreak resulted in 186 cases and 36 deaths.
A third and historically more common example is measles. Measles is a highly contagious, acute viral illness that can lead to serious complications such as pneumonia, encephalitis, and even death. Although not a quarantinable communicable disease, every case of measles in the United States is considered a public health emergency because of its extremely high transmissibility. As a result of high vaccination coverage, measles was declared eliminated (defined as interruption of year-round endemic transmission) from the United States in 2000; however, importations from other countries where measles remains endemic continue to occur, which can lead to clusters of measles cases in the United States in pockets of unvaccinated persons. Of note, an unprecedented outbreak that originated in late December 2014 in Orange County, California resulted in 125 cases; measles cases associated with this outbreak were reported in eight U.S. states, Mexico, and Canada. Between 2010 and 2014, HHS/CDC investigated 91 measles exposures on international or interstate flights, which required time-consuming and labor-intensive location and evaluation of more than 4700 individuals, resulting in the identification of 12 cases of onward transmission. [15]
Global public health authorities have clearly indicated, and evidence has shown, that Ebola, MERS, and measles could spread between countries, and a re-emergence after the current outbreaks are controlled is always a risk. Additionally, although public health responses to measles have become routine over the past decade, the recent unprecedented outbreak in a large U.S. tourist destination with high potential for onward travel by exposed individuals identified greater danger for measles becoming reestablished in the United States in communities with lower rates of immunization. These three examples demonstrate the need for a more timely, efficient, and complete public health response, so that CDC can better protect individuals and prevent the further importation and spread of communicable disease.
This NPRM clarifies and provides greater transparency regarding the tools HHS/CDC uses to identify and respond quickly and effectively to prevent introduction and spread of these and other communicable diseases in the United States. Currently, these processes are governed by standard and internal operating procedures and policies, based upon broad statutory authorities. For instance, it is anticipated that explicit regulatory authority, as proposed in this notice of proposed rulemaking, may lead to quicker and more accurate illness reporting, which would enhance HHS/CDC’s ability to evaluate an ill traveler and assess the public health risk. The current definition of “ill person” does not include the range of signs and symptoms for many of the quarantinable communicable diseases, including Ebola and MERS, nor does it allow for detection of new or emerging communicable diseases. Currently the broader range of signs and symptoms is already requested on a voluntary basis; however, the current regulations do not require mandatory reporting of ill persons as defined by this broader definition, thus requiring HHS/CDC to rely on the voluntary compliance of conveyance operators. Given the grave consequences for mortality and morbidity of introducing and spreading these diseases, a strengthening of this reporting requirement via mandatory reporting according to the revised definition of an ill person, as described in this NPRM, is essential. This is validated by several recent instances of individuals traveling interstate while symptomatic with MERS, Ebola, Lassa fever, and measles. Conducting contact investigations on interstate flights is labor-intensive and often inaccurate and untimely given the current quality of passenger data. This NPRM through proposed section 42 CFR 70.11 would improve HHS/CDC’s ability to receive reports of symptomatic interstate travelers allowing for more efficient evaluation and enabling HHS/CDC to expedite its domestic response activities, (e.g. distributing Passenger Locator Forms) to more quickly and efficiently locate and assess exposed travelers, and mitigate the spread of disease. The proposed updated definition of “ill person” also includes a provision for the CDC Director to revise the symptom definition as needed in response to a newly identified communicable disease; this will greatly enhance HHS/CDC’s ability to respond rapidly to emerging public health threats. By expanding the current regulatory definition to include the requested symptoms, CDC is improving the sensitivity of the system that requires reporting of ill travelers on conveyances, allowing CDC to then make a determination of whether the illness may represent a communicable disease of public health concern.
Since 2007, HHS/CDC has employed basic tools, such as public health travel restrictions list (“Do Not Board list”) to prevent travel by commercial airline of individuals infectious with communicable diseases that pose a public health threat to the traveling public. [16]During the 2014-2016 Ebola epidemic, HHS/CDC revised the criteria for use of Federal travel restrictions to address the need to prevent travel by persons potentially exposed to Ebola or other communicable diseases but not yet considered contagious. The updated criteria provided HHS/CDC with greater flexibility to control the movement of persons who pose a public health threat during travel and to apply Federal travel restrictions in support of outbreak control. In certain circumstances, HHS/CDC has allowed people contagious with or exposed to serious communicable diseases to travel interstate if this can be done in a manner that does not expose the public (e.g., by private vehicle). However, the needs of the individual to engage in travel must be carefully weighed against the public health risk due to the potential lack of public health oversight, especially during travel over long distances or crossing multiple states. For this reason, during the 2014-2016 Ebola epidemic, HHS/CDC recommended against long-distance travel by private vehicle for people with certain types of exposures to Ebola. State and local public health authorities, relying on their own legal processes, enforced these recommendations by imposing their own movement restrictions on individuals potentially exposed to Ebola. While HHS/CDC could similarly impose movement restrictions for individuals reasonably believed to be infected with a quarantinable communicable disease through the issuance of a Federal order for isolation, quarantine, or conditional release, codifying in regulation a separate, formal process to issue interstate travel permits for individuals subject to controlled movement allows for greater transparency and public understanding of what actions HHS/CDC may take to condition an individual’s travel on the observance of public health measures to assure the safety of other travelers and communities.
In the last century, 60% of newly identified infectious diseases in humans globally were zoonotic (transmitted from animals to humans). As mentioned above, evidence indicates that both MERS and Ebola are associated with animal reservoirs (camels and bats, respectively). It is possible any future outbreaks may be linked to animal sources for which an emergency ban on certain animals or cargo (e.g., animal products) would be necessary to protect the public. In the past, HHS/CDC has issued import embargoes either through publication of an interim final rule (e.g., 68 FR 62353 (Nov. 4, 2003) (imposing restrictions on African rodents)) or through issuance of an emergency order under the authority of 42 CFR 71.32(b) (allowing for the application of public health measures to arriving carriers and animals, articles, or things found onboard such arriving carriers) (See http://www.cdc.gov/sars/media/civet-ban.html).
Codifying in regulation a provision explicitly relating to HHS/CDC’s ability to impose an import embargo provides greater transparency and will greatly enhance HHS/CDC’s ability to protect the public from ongoing hazardous importations. We note that while proposed § 71.63 serves to clarify CDC’s authority to temporarily ban certain imports, this is not a new authority and will not alter current CDC practices. HHS/CDC will continue to coordinate in advance with other Federal agencies that have overlapping authority, as may be necessary to implement and enforce this provision.
Finally, this NPRM contains due process provisions (requirements relating to administrative records, quarantine, isolation, conditional release, medical examination, and agreements; authorization for payment for medical care and treatment; and an explanation of applicable criminal penalties) which are intended to inform the U.S. public of what steps HHS/CDC might take to protect public health during an outbreak while safeguarding the rights of the individual. Although these processes have been implemented through internal standard operating procedures, these procedures have not been codified, explicitly set forth in regulation, and made publicly available until today. These provisions are needed to provide transparency and assure the traveling public and any individual potentially placed under a Federal public health order that HHS/CDC will protect their individual liberties.
The provisions in this NPRM describe the regulatory activities that HHS/CDC may undertake to reduce and mitigate the risk of outbreaks of Ebola, MERS, measles, and other communicable diseases in the United States. Greater transparency and public understanding of its processes, authorities, and procedures, will allow HHS/CDC to respond more effectively to these public health emergencies.
V. Ongoing Efforts With U.S Department of Homeland Security (DHS)/U.S. Customs and Border Protection (DHS/CBP) To Improve Passenger Data CollectionBack to Top
CDC is currently working with DHS/CBP to update existing DHS/CBP regulations that will require the electronic collection and submission of additional passenger and crew contact information to the Advance Passenger Information System (APIS) which would streamline the collection of additional data to minimize the burden on airline operators and travelers. We also plan to work with DHS/U.S. Coast Guard (USCG) to develop a comparable electronic data collection mechanism for vessels and their passengers and crew. Therefore this NPRM also informs airline and vessel industry, as well as travelers that HHS/CDC is working with DHS on expanding the data elements currently required and collected via APIS (e.g., seat or cabin number, primary and secondary phone numbers, address information, and email address) that would be reported to CBP regarding passengers and crew on applicable international flights and vessel voyages. These data and additional contact information collected by DHS would then be shared with HHS/CDC as necessary for use in public health contact tracing. We have included the chart below to reflect the data elements of public health interest that are collected under current CDC manifest order practice, which HHS/CDC seeks to codify through this regulation.
| Currently required data elements of public health interest | DHS/CBP-APIS 17 | CDC—manifest order |
|---|---|---|
| Full name (last, first, and, if available, middle or others) | X | X |
| Date of Birth | X | X |
| Sex | X | X |
| Country of Residence | X | X |
| If a passport is required; passport number, passport country of issuance, and passport expiration date | X | X |
| Travel document information | X | X |
| Name of Airline | X | X |
| Flight number | X | X |
| City of departure | X | X |
| Departure date | X | X |
| City of arrival | X | X |
| Arrival date | X | X |
| Address while in the United States (number and street, city, state, and zip code), except that U.S. citizens and lawful permanent residents will provide address of permanent residence in the U.S. (number and street, city, state, and zip code; as applicable) | (18) | X |
| Primary contact phone number to include country code | X | |
| Secondary contact phone number to include country code | X | |
| Email Address | X | |
| Seat or Cabin Number | X |
V. Summary of Notice of Proposed RulemakingBack to Top
A. Updates to Part 70
1. § 70.1 General Definitions
Section 70.1 contains the definitions used in this NPRM. The NPRM proposes new or updated definitions to be consistent with modern quarantine concepts and current medical and public health principles and practice.
Apprehension
Under section 361(d)(1) of the PHS Act (42 U.S.C. 264(d)(1)), HHS/CDC may promulgate regulations that provide for the apprehension and examination of any individual reasonably believed to be infected with a quarantinable communicable disease in a qualifying stage. In addition, HHS/CDC must reasonably believe that the individual is moving or about to move between states or constitutes a probable source of infection to others who may be moving between states. Thus, HHS/CDC believes that it is important to define for the public what is meant by the term “apprehension.” Apprehension means the temporary taking into custody of an individual or group for purposes of determining whether quarantine, isolation, or conditional release is warranted.
Although each instance is unique, an apprehension will typically occur at the request of a state or local health department or in other time-sensitive situations, such as at a U.S. port of entry, where it is necessary for HHS/CDC to take immediate action to protect public health. The factors that may give rise to an apprehension are discussed in detail in the preamble section discussing the definition of “reasonably believed to be infected, as applied to an individual.” When an apprehension occurs, the individual is not free to leave or discontinue his/her discussion with an HHS/CDC public health or quarantine officer. In some cases, an apprehension may last from twenty minutes to one to two hours if, for instance, based on a public health assessment, HHS/CDC is able to quickly rule out the presence of a quarantinable communicable disease. In certain circumstances, the individual may remain apprehended pending confirmation that he or she is not infected or not reasonably believed to be infected with a quarantinable communicable disease. If it is necessary to issue the individual a Federal order for quarantine, isolation, or conditional release, the individual will remain apprehended pending the service of the written order. The factors that may give rise to an order for quarantine, isolation, or conditional release are discussed in detail in the preamble section discussing the definition of “reasonably believed to be infected, as applied to an individual.” Based on past experience, HHS/CDC believes that a written Federal order may be served to an individual within 24-48 hours of an apprehension. These timeframes are merely offered as guidance and HHS/CDC believes that the facts and circumstances of each case will dictate the expected length of an apprehension. Generally, however, HHS/CDC does not expect that the typical public health apprehension will last longer than 72 hours. It is not HHS/CDC’s intent through this definition to allow for extended apprehensions absent the issuance of a Federal order for quarantine, isolation, or conditional release. HHS/CDC requests public comment concerning the expected apprehension period (no longer than 72 hours), and whether there are any public concerns with the absence of a specific maximum apprehension period in the regulation.
Communicable Period
HHS/CDC is proposing to revise the definition of communicable period in part 70. As listed in the table above, under the new definition, communicable period would mean the period during which an infectious agent may be transmitted either directly or indirectly from an infected individual to another individual. Under section 361 (b) and (d) of the Public Health Service Act, to authorize the quarantine, isolation, or conditional release of any individual traveling interstate, HHS/CDC must reasonably believe that an individual is infected with a quarantinable communicable disease in a qualifying stage. 42 U.S.C. 264(b) and (d)(1). As defined by the statute, a “qualifying stage” means that the communicable disease is in “a precommunicable stage, if the disease would be likely to cause a public health emergency if transmitted to other individuals” or “a communicable stage.” Thus, HHS/CDC believes that it is necessary to provide a clear definition for what it means for an individual to be in the communicable stage of a communicable disease. HHS/CDC’s proposed revised definition is consistent with how this term is commonly understood in the public health community.
There are numerous resources to describe the communicability of specific diseases. CDC’s Health Information for International Travel (also known as the Yellow Book) provides the public with general guidance regarding the expected length of communicability for many quarantinable communicable diseases. The most current version is available on CDC’s Web site. For more information, please see http://wwwnc.cdc.gov/travel/yellowbook/2016/table-of-contents.
Agreement
HHS/CDC is proposing a definition for “agreement” which refers to an agreement entered into between the CDC and an individual expressing agreement between the parties that the individual will observe public health measures authorized under this part, as the CDC considers reasonably necessary to protect the public’s health, including quarantine, isolation, conditional release, medical examination, hospitalization, vaccination, and treatment. An explanation of the reasons for why HHS/CDC is including a regulatory provision explicitly allowing for agreements is discussed in detail in the preamble section explaining proposed § 70.8. HHS/CDC believes that the proposed definition is consistent with public health practice and common usage.
Contaminated Environment
HHS/CDC is proposing to define a contaminated environment as meaning the presence of an infectious agent on a surface, including on inanimate articles, or in a substance, including food, water, or in the air. Exposure to a contaminated environment is one method through which an individual may become infected with a communicable disease. Thus, HHS/CDC believes that it is important to define this term for transparency and to enhance the public’s understanding of HHS/CDC’s practices. HHS/CDC believes that the term is being defined consistently with public health practice and common usage.
Conditional Release
HHS/CDC is proposing to define conditional release to mean “surveillance” as that term is proposed in 42 CFR 71.1 and update the definition to include public health supervision through in-person visits by a public health official (or designee), telephone, or through electronic or internet-based monitoring as that term is defined. Surveillance under § 71.1 is currently defined as temporary supervision by a public health official (or designee) of an individual or group, who may have been exposed to a quarantinable communicable disease, to determine the risk of disease spread. HHS/CDC is proposing to expand the definition of conditional release to clarify that it may include electronic or internet-based monitoring in addition to in-person visits by a public health official or telephone reporting by the individual under a conditional release order. A proposed definition for electronic or internet-based monitoring has been included as part of this proposal and is discussed below. In general, such monitoring may include electronic or internet-based systems, such as video chat and voice calls from computers, tablets and mobile devices. This language is intended to be broad and would apply to any new or existing technologies that would allow for the public health supervision and monitoring of an individual under a conditional release order.
Electronic or Internet-Based Monitoring
HHS/CDC has proposed a definition for “electronic or internet-based monitoring” that defines this term as referring to mechanisms or technologies allowing for the temporary public health supervision of an individual under conditional release, including electronic mail, SMS texts, video conference or webcam technologies, integrated voice-response systems, entry of information into a web-based forum, wearable tracking technologies, and other mechanisms or technologies as determined by the Director or supervising health authority. HHS/CDC specifically solicits comment regarding whether this proposed definition is sufficiently broad to apply to any new or existing technologies that would allow for the public health supervision and monitoring of an individual under a conditional release order. HHS/CDC also solicits comment regarding whether the proposed definition raises any privacy implications for an individual who is reasonably believed to be infected with a quarantinable communicable disease and who is subject to a conditional release order.
Ill Person
HHS/CDC is including a proposed definition of “ill person” under part 70 to facilitate identification of communicable diseases of public health concern. Changes in the ill person definition, including the revised temperature threshold and inclusion of persistent diarrhea and vomiting, are particularly aimed at improving HHS/CDC’s ability to detect Ebola. The NPRM definition of “ill person” focuses on the signs and symptoms of communicable diseases of public health concern to ensure such diseases are recognized and reported.
However, HHS/CDC is also including a provision in this NPRM to allow it to include additional signs and symptoms of illness in case our understanding of the recognizable symptoms of communicable diseases of public health concern, such as Ebola, may change or to respond to communicable diseases that may emerge as future concerns. Notice of such additional signs and symptoms will be published in the Federal Register.
HHS/CDC has crafted the proposed definition of “ill person” in such a way that it should be understood by non-medically trained crewmembers and used to discern illnesses of public health interest that HHS/CDC would like to be made aware of according to 42 CFR 70.4 from those that it does not (e.g., common cold), while more closely aligning the definition with the symptoms reporting guidelines published by ICAO in Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation. To further assist flight crewmembers (and vessel crewmembers under part 71) in identifying individuals with a reportable illness, HHS/CDC provides the following in-depth explanations and examples of the communicable diseases that such signs and symptoms might indicate. Note that these explanations also apply to the definition of “ill person” under part 71.
1. Fever: This term means that the person has a measured temperature of 100.4 °F (38°C) or greater, feels warm to the touch, or gives a history of feeling feverish. While a measured temperature is the preferable and more accurate method to determine whether a person has a fever, it is not always possible to obtain. The measured temperature also may not reflect the presence of a recent fever, for example, if the individual has taken a fever-reducing medication. For these reasons, the revised “ill person” definition includes other methods that may be used by crewmembers as proxies for a measured temperature. If it is not feasible or advisable to touch the individual or if the individual does not disclose a history of feeling feverish, then, while not definitive, the observer should consider his/her appearance, such as having a flushed face, glassy eyes, or chills as possible indications of the presence of a fever. A self-reported history of feeling feverish is included in the event that the ill person has taken medication that would lower the measured temperature or if the fever fluctuates as part of the natural course of the disease.
2. Skin rash: This term means that the individual has areas on the skin with multiple red bumps; red, flat spots; or blister-like bumps filled with fluid or pus that are intact or partly crusted over. The rash may be discrete or may run together, and may include one area of the body, such as the face, or more than one area. The presence of skin rash, along with fever, may indicate that the traveler has measles, rubella (German measles), varicella (chickenpox), meningococcal disease, or smallpox.
3. Difficulty breathing: This term means that the individual is gasping for air, is unable to “catch” his/her breath, is breathing too fast and shallow to get enough air, or cannot control his/her own secretions. These symptoms may be apparent or self-reported if not obvious. Difficulty breathing, along with fever, may indicate a traveler has tuberculosis, diphtheria, influenza with pandemic potential, or a severe acute respiratory syndrome.
4. Persistent cough: This term means that the cough is frequent and severe enough that it catches the attention of the crewmember, or the individual or another passenger voices concern about it. Persistent cough, along with fever, may indicate the traveler has pertussis/whooping cough (vomiting may occur at the end of a coughing fit), tuberculosis, severe acute respiratory syndrome, or influenza with pandemic potential.
5. Decreased consciousness or confusion of recent onset: This term means that the individual is not fully aware of his/her surroundings or may be unusually difficult to awaken. The individual may appear to be confused or disoriented. Decreased consciousness, along with fever, may indicate the traveler has meningococcal disease, another serious neurological infection, or serious infection in another body system.
6. Bruising or bleeding (without previous injury): This term means that the person has noticeable and unusual bruising or bleeding from gums, ears, nose or areas on skin for which there is no obvious explanation. Unexplained bruising or bleeding, along with fever, may indicate the person has a hemorrhagic fever, such as Ebola, or plague.
7. Persistent diarrhea: This term means that the diarrhea is frequent and severe enough that the air crewmember notices, for example, that the person has been to the restroom numerous times, or the individual or another passenger voices concern about it. Persistent diarrhea may indicate the person has a foodborne or waterborne infection such as norovirus or cholera, or another serious communicable disease, such as Ebola. Many infections that cause persistent diarrhea can be spread easily from person to person, either directly or indirectly through food or water, and cause large outbreaks.
8. Persistent vomiting: This term means that the individual has vomited two or more times (not due to air or sea sickness) and either expresses concern to the air/vessel crew or comes to the attention of others onboard (air/vessel crew or passengers). Persistent vomiting may indicate the person has a foodborne or waterborne infection such as norovirus, or another serious communicable disease, such as Ebola.
9. Headache with stiff neck: This term means that the individual is self-reporting a headache accompanied by difficulty moving his/her neck. These symptoms may indicate that the individual has bacterial meningitis, such as meningococcal meningitis. Meningococcal meningitis has a high death rate and a significant proportion of survivors have residual impairments, such as deafness or injury to the brain. Individuals in close contact with ill persons with meningococcal disease are at elevated risk for contracting the disease.
10. Obviously unwell: HHS/CDC has included this description into the proposed definition of “ill person” as it is used in ICAO guidelines to aid crewmembers in the identification of symptoms of communicable disease. See Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation.
Indigent
CDC conducts a mandatory reassessment 72 hours after the service of all Federal orders for quarantine, isolation, or conditional release. A medical review is part of the administrative appeals process whereby an individual under a Federal order may request a separate medical review of his/her case after the mandatory reassessment is complete. HHS/CDC is defining the term “indigent” for purposes of appointing a medical representative for indigent individuals placed under a Federal order of quarantine, isolation, or conditional release who request a medical review and appointment of a medical representative.
An indigent individual is defined as one whose annual family income is below 150% of the applicable poverty guidelines updated periodically in the Federal Register by the U.S. Department of Health and Human Services under the authority of 42 U.S.C. 9902(2) or liquid assets totaling less than 15% of the applicable poverty guidelines if no income is earned. The poverty guidelines are updated periodically by HHS and are used for determining eligibility for a number of Federal, state, local, and private programs. The poverty guidelines for 2016 are published at 81 FR 4036 (Jan. 25, 2016). The medical review process is explained in more detail below. CDC specifically requests public comment on whether the use of this standard definition is an appropriate threshold to determine whether an individual cannot afford representation and therefore should be appointed a medical representative at the government’s expense.
Medical Examination
Under section 361(d)(1) of the PHS Act (42 U.S.C. 264(d)(1)), HHS/CDC may promulgate and enforce regulations concerning the apprehension and examination of any individual reasonably believed to be infected with a quarantinable communicable disease in a qualifying stage who is, or is reasonably expected to be, moving or about to be moving between states or constitutes a probable source of infection to others who may be moving between states. Thus, HHS/CDC believes that it is important to define for the public what is meant by a medical examination. Under this NPRM, we define Medical examination to mean the assessment of an individual by an authorized health worker to determine the individual’s health status and potential public health risk to others and may include the taking of a medical history, a physical examination, and the collection of human biological samples for laboratory testing. Medical examination may be authorized as part of a Federal order for quarantine, isolation, or conditional release. The process for ordering a medical examination is explained in more detail in the portion of the preamble discussing that substantive provision at § 70.12.
Medical Representative
HHS/CDC is providing an opportunity for any individual under a Federal order of quarantine, isolation, or conditional release to request a medical review. As part of this process, the individual under the Federal order may choose anyone to represent him/her at the medical review at his/her own expense or to represent himself/herself. However, in the case of an individual who is indigent and cannot afford his/her own representative, HHS/CDC will appoint at government expense a medical representative to assist the indigent individual with the presentation of evidence during the medical review. Appointments by HHS/CDC will be made only if the individual qualifies as an indigent, requests a medical review, and specifically requests the appointment of a medical representative. Again, individuals who do not qualify as indigent may choose to be represented by anyone at their own expense or to represent themselves at the medical review. Because HHS/CDC views the medical review process as a medical fact-finding, it has defined the “medical representative” in terms of the relevant medical qualifications. Medical representative means a physician, nurse practitioner, or similar medical professional qualified in the diagnosis and treatment of infectious diseases who is appointed by the HHS Secretary or CDC Director to assist an indigent individual under Federal quarantine, isolation, or conditional release with a medical review. The medical representative’s role will be to assist the indigent individual with the examination of witnesses and the presentation of factual and scientific evidence during the medical review. The medical representative and the medical reviewer will not be the same individual. Individuals who do not qualify as indigent may choose to be represented by anyone at their own expense or to represent themselves at the medical review.
Medical reviewer means a physician, nurse practitioner, or similar medical professional qualified in the diagnosis and treatment of infectious diseases who is appointed by the HHS Secretary or CDC Director to conduct a medical review. The medical reviewer may be an HHS or HHS/CDC employee, but only if the employee differs from the HHS/CDC official who issued the Federal order for quarantine, isolation, or conditional release. The medical reviewer’s role will be to review the medical or other evidence presented, make medical or scientific findings of fact, and issue a recommendation to the CDC Director concerning whether the quarantine, isolation, or conditional release should be continued, rescinded, or modified. The medical reviewer and the medical representative will be different individuals.
Non-Invasive
The definition of non-invasive has been added to this NPRM to provide the public with reasonable assurances and expectations regarding what measures may be employed as part of a public health risk assessment or following reporting of an ill traveler. We define non-invasive as “procedures conducted by an authorized health worker or other individual with suitable training and includes the visual examination of the ear, nose, and mouth; temperature assessments using an ear, oral, or cutaneous or noncontact thermometer or thermal imaging; auscultation; external palpation; external measurement of blood pressure; and other procedures not involving the puncture or incision of the skin or insertion of an instrument or foreign material into the body or a body cavity, except the ear, nose, or mouth.” HHS/CDC specifically requests comment concerning this definition including whether the definition aligns with common perceptions of what constitutes non-invasive procedures that may be conducted outside of a traditional clinical setting.
Precommunicable Stage
Under section 361(d) of the Public Health Service Act, to authorize the quarantine, isolation, or conditional release of an individual traveling interstate, CDC must reasonably believe that the individual is infected with a communicable disease in a qualifying stage. 42 U.S.C. 264(d)(1). As defined by the statute, a “qualifying stage” means that the communicable disease is in “a precommunicable stage, if the disease would be likely to cause a public health emergency if transmitted to other individuals” or “a communicable stage.” Thus, HHS/CDC believes that it is necessary to define the precommunicable stage of a communicable disease to adequately inform the public of when quarantine, isolation, or conditional release may be authorized. HHS/CDC defines precommunicable stage to mean the stage beginning upon an individual’s earliest opportunity for exposure to an infectious agent and ending upon the individual entering or reentering the communicable stage of the disease or, if the individual does not enter the communicable stage, the latest date at which the individual could reasonably be expected to have the potential to enter or reenter the communicable stage. For instance, a patient diagnosed with multidrug-resistant or extensively drug-resistant tuberculosis who is not currently infectious but has not been adequately treated for the disease and is thus considered to be at high risk of relapse to an infectious state would be in the “precommunicable stage” of the disease. For clarity, and to be consistent with statutory language, we have also updated the definition of “incubation period” to mean the time from the moment of exposure to an infectious agent that causes a communicable disease until signs and symptoms of the communicable disease appear in the individual or for a quarantinable communicable disease the precommunicable stage of the disease.
While it is important that HHS/CDC maintain flexibility to evaluate each case individually regarding the length of quarantine, CDC’s Health Information for International Travel (also known as the Yellow Book) provides the public with general guidance regarding the expected incubation period for many quarantinable communicable diseases. The most current version is available on CDC’s Web site. For more information, please see http://wwwnc.cdc.gov/travel/yellowbook/2016/table-of-contents.
Public Health Emergency
Under section 361(d) of the Public Health Service Act, in order to authorize the quarantine, isolation, or conditional release of any individual traveling interstate, CDC must reasonably believe that an individual is infected with a communicable disease in a qualifying stage. 42 U.S.C. 264(d)(1). As defined by this subsection, a “qualifying stage” means that the communicable disease is in “a precommunicable stage, if the disease would be likely to cause a public health emergency if transmitted to other individuals” or “a communicable stage.” 42 U.S.C. 264(d)(2). While the phrase “public health emergency” also appears under section 319 of the Public Health Service Act (42 U.S.C. 247d(a)), the use of the same phrase in both sections 319 and 361(d)(2) are not necessarily synonymous. Accordingly, HHS/CDC felt it was important to define “public health emergency” as used under section 361(d)(2) to provide the public with a clear understanding of HHS/CDC’s authority for interstate quarantine, isolation or conditional release. Public health emergency as used in this part means any communicable disease event as determined by the CDC Director with either documented or significant potential for regional, national, or international communicable disease spread or that is highly likely to cause death or serious illness if not properly controlled; or any communicable disease event described in a declaration by the Secretary pursuant to § 319(a) of the Public Health Service Act (42 U.S.C. 247d(a)); or any communicable disease event the occurrence of which is notified to the World Health Organization, in accordance with Articles 6 and 7 of the International Health Regulations, as one that may constitute a Public Health Emergency of International Concern; or any communicable disease event the occurrence of which is determined by the Director-General of the World Health Organization, in accordance with Article 12 of the International Health Regulations, to constitute a Public Health Emergency of International Concern; or any communicable disease event for which the Director-General of the World Health Organization, in accordance with Articles 15 or 16 of the International Health Regulations, has issued temporary or standing recommendations for purposes of preventing or promptly detecting the occurrence or reoccurrence of the communicable disease. HHS/CDC specifically requests public comment on this definition and its utility in identifying communicable diseases that “would be likely to cause a public health emergency if transmitted to other individuals” under 42 U.S.C. 264(d)(2)(B).
Public Health Prevention Measures
Under this NPRM, Public health prevention measures means the assessment of an individual through non-invasive procedures and other means, such as observation, questioning, review of travel documents, review of other available records to determine the individual’s health status and potential public health risk to others (i.e.,passenger screening). HHS/CDC believes that this definition is consistent with how public health risk assessments are generally conducted at U.S. ports and other locations, including by HHS/CDC personnel. HHS/CDC is publishing this definition to describe its authority to conduct public health prevention measures and is not effecting a change in operations.
Qualifying Stage
Under this NPRM, “qualifying stage” means the communicable stage of a quarantinable communicable disease, or the precommunicable stage of the quarantinable communicable disease, but only if the quarantinable communicable disease would be likely to cause a public health emergency if transmitted to other individuals. This NPRM also separately defines “communicable stage” and “precommunicable stage.” HHS/CDC believes that these definitions are consistent with public health practice and the requirements of 42 U.S.C. 264(d)(2).
Reasonably Believed To Be Infected, as Applied to Individuals
HHS/CDC is including this definition in this NPRM for transparency and so that the public understands the factors taken into consideration when HHS/CDC makes a determination to issue a Federal order for quarantine, isolation, or conditional release. By adding this definition, HHS/CDC is not changing its operations, but rather is codifying and providing an explanation to the public. Under this NPRM, reasonably believed to be infected, as applied to an individual, means specific articulable facts upon which a public health officer could reasonably draw the inference that an individual has been exposed, either directly or indirectly, to the infectious agent that causes a quarantinable communicable disease, as through contact with an infected person or an infected person’s bodily fluids, a contaminated environment, or through an intermediate host or vector, and that as a consequence of the exposure, the individual is or may be harboring in the body the infectious agent of that quarantinable communicable disease. HHS/CDC believes that this standard is consistent with the legal requirements of the statute, public health practice, and long-standing historical practice concerning the quarantine and isolation of individuals.
The determination as to whether an individual is “reasonably believed to be infected,” as defined in this NPRM, with a quarantinable communicable disease in a qualifying stage is made on a case-by-case basis. Notwithstanding, the following illustrative examples are provided to help explain to the public when facts or circumstances may exist giving rise to a reasonable belief that an individual is infected with a quarantinable communicable disease in its qualifying stage. These include: Clinical manifestations in the individual consistent with those of a quarantinable communicable disease; suspected contact with cases or suspect cases of individuals infected with a quarantinable communicable disease in its communicable stage; host susceptibility to a quarantinable communicable disease combined with opportunity for exposure; travel to countries and places where transmission of a quarantinable communicable disease has likely occurred; reports of the individual exhibiting illness or symptoms consistent with those of a quarantinable communicable disease; or other evidence of possible infection, including exposure to the infectious agent that causes a quarantinable communicable disease. These factors are meant to be illustrative and provide only general guidance. HHS/CDC specifically solicits public comment regarding this definition, in particular, whether the definition aligns with established public health practice regarding the handling of individuals exposed to or infected with communicable diseases.
2. § 70.5 Requirements Relating to Travelers Under a Federal Order of Isolation, Quarantine, or Conditional Release
This provision of the NPRM proposes to replace the previous § 70.5 Certain Communicable Diseases; special requirements that imposes an interstate travel permit requirement for persons in the communicable stage of cholera, plague, smallpox, typhus, or yellow fever. The existing provision also prohibits conveyance operators from “knowingly” accepting for transportation any individual in the communicable stage of any of the specified diseases or in violation of the terms of the travel permit.
Under this NPRM, any individual under a Federal order, or agreement, of isolation, quarantine, or conditional release for a quarantinable communicable disease, as specified by Executive Order, may be prohibited from traveling in interstate traffic, unless the individual has received a written travel permit issued by HHS/CDC. The term “interstate traffic” is currently defined in HHS/CDC regulations at 42 CFR 70.1 and includes movement from a point of origin in any state or possession to a point of destination in any other state or possession. This provision also applies to an “agreement” for isolation, quarantine, or conditional release. An individual must retain the travel permit in his/her possession and comply with the conditions for travel set forth in the permit.
If an individual is denied an application for a travel permit, the denial will be issued in writing. The letter of denial will include the reasons for the denial as well as detailed instructions on whom to contact for questions, including name, address, and telephone number, as well as how to submit an appeal. Individuals who wish to contest HHS/CDC’s determination will have 10 calendar days after receiving the letter of denial to submit an appeal. The appeal must be submitted in writing to the CDC, stating the reasons for the appeal and showing that there is a genuine and material issue of fact in dispute. Individuals should include also the reference number listed in the notification letter they received. The appeal should be addressed to: Director, Division of Global Migration and Quarantine, ATTN: Travel Restriction and Intervention Activity, Centers for Disease Control and Prevention, 1600 Clifton Road NE., MS E-03, Atlanta, GA 30329. Appeals may also be faxed to HHS/CDC at (404) 718-2158 or emailed to travelrestrictions@cdc.gov.
HHS/CDC will issue a written response to an appeal, which shall constitute final agency action. The appeal will be reviewed and decided upon by an HHS/CDC senior official who will be senior to the employee who issued the initial letter of denial. This appeal process is also applicable to revocations and suspensions of a travel permit.
Conveyance operators are also prohibited from ”knowingly” transporting an individual under a Federal order, or agreement, of isolation, quarantine, or conditional release without a travel permit or someone who is in violation of the terms of a permit. This prohibition only applies in circumstances where the operator would be reasonably considered to know or have knowledge that the individual is under a public health order and requires a travel permit. For instance, if the operator has been informed directly by the CDC, or if DHS, upon the request of CDC, has placed the individual’s name on a Federal public health travel restrictions list (“Do Not Board” (DNB) list)—which would only apply to aircraft operators.
The provisions of this section may also be applied to individuals under a state or local order, or an agreement, (if operators are directly notified by authorities that an individual is under a state or local order) for quarantine, isolation, or conditional release, or to those individuals traveling entirely within a state and to intrastate conveyance operators at the request of a state or local health department or in the event of inadequate local control as determined by the CDC Director under 42 CFR 70.2. In the event that this provision is applied intrastate, CDC will work with the relevant state or local health department of jurisdiction to inform intrastate conveyance operators (e.g., bus operators) on a case-by-case basis of the names of individuals subject to this restriction. The application of these provisions to intrastate travel is authorized under section 361(a) of the Public Health Service Act (42 U.S.C. 264(a)) to the extent that such measures are necessary to prevent the interstate spread of communicable diseases. Specifically, because the statute authorizes the promulgation of regulations that are necessary to “prevent” interstate spread of disease, HHS/CDC may regulate certain activities that occur entirely within a State if those activities present a risk of interstate disease spread, as would occur, for instance, in the event of inadequate local control. This approach is consistent with how courts have interpreted the scope of the Federal government’s authority under the Commerce Clause to the U.S. Constitution. See United States v. Lopez, 514 U.S. 549, 558-559 (1995) (noting that the Commerce Clause authorizes the regulation of the instrumentalities of interstate commerce, or persons or things in interstate commerce, even though the threat to interstate commerce may come only from intrastate activities). This provision is also consistent with HHS/CDC’s Interim U.S. Guidance for the Monitoring and Movement of Persons with Potential Ebola Virus Exposure, published during the 2014-2016 Ebola epidemic (a description of the guidance is available at http://www.cdc.gov/vhf/ebola/hcp/monitoring-and-movement-of-persons-with-exposure.html). HHS/CDC specifically requests public comment on this proposed provision.
HHS/CDC recognizes that the right to engage in travel within the United States is a privilege of national citizenship protected by the Privileges and Immunities Clause of the U.S. Constitution, as well as an aspect of liberty protected by the Due Process Clauses of the Fifth and Fourteenth Amendments. See Jones v. Helms, 452 U.S. 412, 418 (1981). However, this right is not unqualified and travel restrictions based on the threat posed by communicable diseases are valid. See Zemel v. Rusk,381 U.S. 1, 15-16 (1965) (“The right to travel within the United States is of course also constitutionally protected . . . [b]ut that freedom does not mean that areas ravaged by flood, fire or pestilence cannot be quarantined when it can be demonstrated that unlimited travel to the area would directly and materially interfere with the safety and welfare of the area or the Nation as a whole.”). Furthermore, HHS/CDC will afford individuals subject to these travel restrictions with adequate due process through the previously mentioned written appeals process.
This new regulatory provision also serves as an important complement to the public health “Do Not Board” (DNB) list. In June 2007, HHS/CDC and the Department of Homeland Security (DHS) developed a public health DNB list, enabling domestic and international public health officials to request that individuals with communicable diseases who meet specific criteria, including posing a public health threat to the traveling public, be restricted from boarding commercial aircraft arriving into, departing from, or traveling within the United States. See Criteria for Requesting Federal Travel Restrictions for Public Health Purposes, Including for Viral Hemorrhagic Fevers. Available at: https://www.Federalregister.gov/articles/2015/03/27/2015-07118/criteria-for-requesting-Federal-travel-restrictions-for-public-health-purposes-including-for-viral.
The public health DNB list, which is administered by DHS with HHS/CDC’s assistance, is primarily intended to supplement state and local public health measures to prevent individuals who are infectious or at risk of becoming infectious from boarding commercial aircraft. However, because use of the DNB list is limited to commercial aircrafts, the public health protections offered by the DNB list do not extend to vessels, or other forms of interstate transportation, such as trains and buses. Thus, this new provision allows for an enhanced HHS/CDC public health response to quarantinable communicable diseases by establishing a permitting process that restricts interstate travel to modes of conveyance that do not put the public at risk of exposure, and ensures that appropriate public health measures are in place. CDC specifically requests public comment on this provision. In particular, HHS/CDC requests comment on whether stakeholders have concerns regarding the requirement imposed on conveyance operators to not “knowingly” transport individuals under a Federal order and the feasibility of this requirement. HHS/CDC also requests public comment on the application of this provision to individuals under state/local order as well as individuals traveling entirely within a state.
3. § 70.6 Apprehension and Detention of Persons With Quarantinable Communicable Diseases
Through this NPRM, HHS/CDC has proposed to change the text of this provision.
We have modified “infected with a quarantinable communicable disease” to clarify, consistent with the statute’s requirements, that the individual must be in the “qualifying stage” of a quarantinable communicable disease, which we also define. We did this to better align our regulations with the Public Health Service Act which authorizes the “apprehension and examination of any individual reasonably believed to be infected with a [quarantinable communicable] disease in its qualifying stage and (A) moving or about to move from a state to another state; or (B) to be a probable source of infection to individuals who, while infected with such disease in a qualifying stage, will be moving from a state to another state.” See 42 U.S.C. 264(d)(1)(2). The statute’s requirement for interstate movement is reflected in the requirement in § 70.6 that HHS/CDC’s custody of the individual be “for the purposes of preventing the interstate introduction, transmission, or spread of quarantinable communicable diseases.”
4. § 70.10 Public Health Prevention Measures To Detect Communicable Disease
This provision is authorized by the Public Health Service Act. Section 361(a) of the PHS Act (42 U.S.C. 264(a)) authorizes the HHS Secretary to promulgate regulations to prevent the interstate introduction, transmission, and spread of communicable diseases. As previously mentioned, section 361(a) (42 U.S.C. 264(a)) applies broadly to communicable diseases generally and is not limited to those subset of communicable diseases referred to as “quarantinable communicable diseases” for which quarantine, isolation, or conditional release are authorized. Section 361(a) includes the authority to allow for a variety of public health measures in regard to communicable diseases including: Inspection, fumigation, disinfection, sanitation, pest extermination, destruction of animals or articles found to be sources of dangerous infection to human beings, and other measures to protect public health. Specifically, this list of public health actions does not involve taking persons into custody or require reasonable suspicion as a predicate to implementation. In contrast an “apprehension, detention, or conditional release” as used in section 361(b) involves custodial situations and requires, with regard to persons moving between states or U.S. territories, a reasonable belief that the individual is in the qualifying stage of a quarantinable communicable disease.
In addition to being consistent with the requirements of section 361 of the Public Health Service Act, this provision is also consistent with constitutional principles and requirements. For instance, in the analogous situation of an airport security screening, it is well established that the Transportation Security Administration may conduct routine warrantless searches of all carry-on luggage without individualized suspicion because of the compelling government interest involved. See United States v. Doe, 61. F.3d 107, 110 (1st Cir. 1995) (“Routine security searches at airport checkpoints pass constitutional muster because the compelling public interest in curbing air piracy generally outweighs their limited intrusiveness.”); see also Russkai v.Pistole, 775 F.3d 61, 68 (1st Cir. 2014) (noting that transit security screenings are treated as “administrative” or “special needs” searches, which may be conducted, at least initially, without individualized suspicion, a warrant, or probable cause). HHS/CDC believes that the rationale for airport security screenings may be extended to other forms of transportation, e.g., trains and buses, because of the similar “administrative” or special governmental need in preventing interstate communicable disease spread. Public health risk assessments are limited to non-invasive means, as defined in this NPRM, which includes temperature assessments using an ear, oral, cutaneous, or noncontact thermometer, auscultation, external palpation, external measurement of blood pressure, as well as questioning of individuals and review of travel documents. HHS/CDC does not intend through this provision to engage in medical testing of individuals (as would typically occur in a hospital or other clinical setting) at ports of entry or other places where individuals may engage in travel or to collect human biological samples for subsequent laboratory testing.
HHS/CDC’s intent under this provision is to provide for mandatory public health risk assessment and management at ports or other locations where individuals may gather to engage in interstate traffic. However, as in other circumstances where individuals are screened, such as airport security screenings, an individual’s willingness to be screened may be inferred from his or her queueing with other travelers who may be engaging in interstate travel. See United States v. Herzbrun,723 F.2d 773, 775 (11th Cir. 1984) (holding that a passenger consents to an airport security search by presenting himself/herself for boarding and that such consent may not be revoked by simply walking away). Thus, in order to protect interstate travel from communicable disease threats, HHS/CDC intends for this section to apply broadly to all circumstances where individuals may queue with other travelers because certain communicable diseases may be spread from person to person under such circumstances. This includes circumstances where only a certain percentage of travelers may be intending to subsequently engage in interstate travel or, for instance, the individual traveler is intending to engage in foreign travel outside the country as opposed to domestic interstate travel because by queuing in line with others at the airport he or she may expose other travelers intending to engage in interstate travel. HHS/CDC specifically requests public comment on this proposed provision and whether the public has any concerns regarding the mandatory health screening of passengers using non-invasive means as defined in this proposed rule.
During a public health risk assessment, if facts or circumstances are discovered that give rise to a reasonable belief that the individual is infected, as defined under this NPRM, with a quarantinable communicable disease in its qualifying stage, CDC may authorize the quarantine, isolation, or conditional release of the individual. Similarly, an individual’s refusal to be screened may result in quarantine, isolation, or conditional release, but only if sufficient facts and circumstances otherwise exist giving rise to a reasonable belief that the individual is infected with a quarantinable communicable disease in its qualifying stage.
Under section 311 of the PHS Act (42 U.S.C. 243), HHS/CDC may accept state and local assistance in the enforcement of Federal quarantine rules and regulations, though these entities are not obligated to provide such assistance. In appropriate cases, Federal law enforcement agencies may also be able to assist in the enforcement of Federal public health orders. Under section 365 of the PHS Act (42 U.S.C. 268) it shall be the duty of “customs officers” and “Coast Guard officers” to aid in the enforcement of Federal quarantine rules and regulations. “Customs officers” includes U.S. Customs and Border Protection (CBP) officers, U.S. Border Patrol agents, U.S. Immigration and Customs Enforcement (ICE) officers, and U.S. Coast Guard Commissioned, Warrant, and Petty Officers pursuant to 14 U.S.C. 143 and 19 U.S.C. 1401(i).
This section also requires individuals undergoing a public health risk assessment to provide basic contact tracing information which would be used to locate and notify individuals of a potential exposure to a communicable disease. This information would include U.S. and foreign addresses, telephone numbers, email addresses, used to locate and notify an individual. This section would also require that individuals undergoing a public health risk assessment provide additional information that would be used to assess an individual’s health status and make a determination as to whether the individual may pose a public health risk to others. This would include information concerning the individual’s intended destination, health status, and history of travel to places where exposure to communicable disease may have occurred. HHS/CDC specifically requests public comment on this proposed provision to collect additional personal information from screened individuals for the purposes of contact tracing.
On December 13, 2007, HHS/CDC published a notice of a new system of records (SORN) under the Privacy Act of 1974 that is relevant to the activities that would be carried out under a future rule related to collecting, retaining, and disseminating passenger and crew data for public health purposes (72 FR 70867). HHS/CDC accepted public comment on its proposed routine uses of this information at that time. As required under the Privacy Act, in its notice, HHS/CDC described the proposed system of records; the proposed routine uses, disclosures of system data, the benefits and need for this data, agency policies and procedures, restrictions on the use of this information, and, most important, HHS/CDC’s safeguards to prevent unauthorized use. Data collected from travelers, ill persons, and individuals under Federal public health orders will be maintained in accordance with the Privacy Act and the system of records notice regardless of whether the individual is a U.S. citizen or foreign national. More information regarding the storage, maintenance, and routine uses of this information may be found at 72 FR 70867 (Dec. 13, 2007). HHS/CDC will make disclosures from the system of records only with the consent of the subject individual or in accordance with the Privacy Act or its Privacy Act system of records notice. As a matter of practice, HHS/CDC applies these same requirements and protections afforded by its Privacy Act system of records notice to non-U.S. persons whose personal information is collected and maintained in this system of records.
5. § 70.11 Report of Death or Illness Onboard Aircraft Operated by Airline
This NPRM specifies that the pilot in command of an aircraft operating on behalf of an airline who conducts a commercial passenger flight in interstate traffic under a regular schedule, shall report as soon as practicable to the HHS/CDC the occurrence onboard of any deaths or ill persons among passengers or crew and take such measures as HHS/CDC may direct to prevent the potential spread of the communicable disease, provided that such measures do not affect the aircraft’s airworthiness or safety of flight operations. While this provision specific to interstate travel is new to the regulation, the reporting of deaths or illnesses among passengers and crew has been a long-established practice for flights arriving into the United States. Between 2010 and 2015, per year on average, HHS/CDC received about 175 illness and 10 death reports on aircraft and about 220 illness reports and 115 death reports from vessels. In light of recent events, such as the outbreaks of Ebola, measles and MERS, and the possibility that symptomatic, infectious individuals may board interstate flights, HHS/CDC believes it important to introduce this section to ensure that domestic flights report directly to HHS/CDC.
This proposed section of the rule applies to aircraft and does not apply to other forms of transportation, such as buses and trains, because air travel generally carries an especially high risk of rapid transmission and dispersal of communicable disease as air travelers are able to easily connect to other flights and move around the country in just a few hours. Furthermore, if a traveler developed symptoms of a serious communicable disease onboard a bus or train, it might be easier for the bus or train operator to segregate or remove the ill person than onboard an aircraft. CDC also believes that it is easier for a local public health authority to respond to reports of an ill person onboard a bus or train traveling through its jurisdiction, even if ultimately on an interstate journey, than it would be for the same authority to respond to reports of an ill person on an aircraft. Furthermore, if the requirement were extended to interstate buses and trains, HHS/CDC believes that implementing this provision would be overly burdensome.
HHS/CDC further notes that it is making no changes to its existing regulatory requirement at 42 CFR 70.4 which states that the master of a vessel or person in charge of any conveyance engaged in interstate traffic on which a case or suspected case of communicable disease develops shall, as soon as practicable, notify the local health authority. Under this NPRM, the pilot in command of an aircraft operating on behalf of an airline who submits the ill person report to HHS/CDC will not be required to also submit a report to the local health authority. HHS/CDC will continue to share public health information with state and local health departments through electronic disease reporting networks such as the Epidemic Information Exchange (Epi-X), HHS/CDC’s secure, web-based system. CDC may also notify local authorities via a Health Alert Notice (HAN), and when necessary, via phone calls, email, or other direct communication.
If finalized as proposed, in implementing this provision, an airline should establish a notification system sufficient to ensure that any death or ill person, as defined, that is made known to the pilot in command is reported to CDC either through the quarantine station of jurisdiction for the destination airport or the CDC Emergency Operations Center (EOC), where possible, at least one hour before arrival. The EOC serves an important triage function within HHS/CDC and operates 24-hours a day. CDC’s EOC also is capable of quickly contacting the relevant state and local health authority and quarantine station of jurisdiction as well as assembling the necessary subject-matter experts for purposes of conducting a public heath investigation.
This proposed provision is intended to provide airlines with flexibility regarding the exact routing of reports of deaths or ill persons, as defined. Thus, this NPRM explicitly authorizes airlines to develop and adopt a notification system that relays information from the pilot in command to CDC’s EOC through a designated official of the airline. This may be accomplished by the pilot-in-command making a report of a death or ill person to the U.S. Department of Transportation (DOT)’s Federal Aviation Administration (FAA) air traffic control (ATC) facility. In such cases, the DOT/FAA will notify the CDC’s EOC via DOT/FAA’s Domestic Events Network (DEN), of the report. However, ATC channels will not be used by CDC or airlines for any subsequent coordination regarding the public health response that follows the initial report, unless no other reasonable alternative exists. ATC channels are open radio frequencies whose primary purpose is ensuring the safe and efficient movement of aircraft in the National Airspace System, and any personal health information broadcast over them may be overhead by any person with the appropriate equipment.
HHS/CDC believes that an airline is in the best position to develop a notification system, because airlines presumably already have such systems in place for reporting of deaths or illnesses under CDC’s existing regulations in 42 CFR parts 70 and 71 and to the relevant authorities for international flights. HHS/CDC, in coordination with DOT/FAA, may issue additional guidance to airlines regarding recommended procedures for the domestic reporting to the CDC’s EOC of any death or ill person made known to the pilot in command. HHS/CDC will consider the adoption and implementation by an airline of a notification system as a measure of an airline’s compliance with this provision.
6. § 70.12 Medical Examinations
Under section 361(d)(1) of the PHS Act (42 U.S.C. 264(d)(1)), HHS/CDC may promulgate and enforce regulations concerning the apprehension and examination of any individual reasonably believed to be infected with a quarantinable communicable disease in a qualifying stage e. In addition, HHS/CDC must reasonably believe that the individual is moving or about to move between states or constitutes a probable source of infection to others who may be moving between states. Statutory support for medical examinations may be found directly under 42 U.S.C. 264(d)(1) which authorizes regulations allowing the “apprehension and examination” of any individual reasonably believed to be infected with a quarantinable communicable disease in a qualifying stage. Thus, HHS/CDC believes it is important to make this process more transparent and explicit. Accordingly, HHS/CDC is clarifying that the requirement for a medical examination by an authorized health worker may be included as part of a Federal order for quarantine, isolation, or conditional release. We specifically request public comment on this proposed provision and whether there are any concerns regarding the proposed practice to issue Federal orders before a medical examination has taken place.
HHS/CDC will promptly arrange for a medical examination to be conducted in circumstances where such an examination is necessary to confirm the presence or absence of infection with a quarantinable communicable disease. A medical examination will typically occur in a hospital setting and be performed by clinical staff that will have primary responsibility for the patient’s medical care and treatment. HHS/CDC will consult with hospital staff regarding the public health management of the case. A medical examination may include the taking of a medical history, a physical examination, and taking of laboratory samples.
The determination as to whether a medical examination may be necessary in any given circumstances is by its nature highly fact dependent. Notwithstanding, the following illustrative examples are provided to help explain to the public when facts or circumstances may exist giving rise to a need for a medical examination. These include the following circumstances: Clinical manifestations in the individual consistent with those of a quarantinable communicable disease; suspected contact with cases or suspect cases of individuals infected with a quarantinable communicable disease in its communicable stage; host susceptibility to a quarantinable communicable disease combined with opportunity for exposure; travel to countries and places where transmission of a quarantinable communicable disease has likely occurred; reports of the individual exhibiting illness or symptoms consistent with those of a quarantinable communicable disease; or other evidence of possible infection, including exposure to the infectious agent that causes a quarantinable communicable disease. These factors are meant to be illustrative and provide only general guidance.
7. § 70.13 Payment for Care and Treatment
Under this proposed section, HHS/CDC may pay for the care and treatment of individuals subject to apprehension, medical examination, quarantine, isolation, and conditional release after the exhaustion of all third party payments. This section implements § 322 of the Public Health Service Act (42 U.S.C. 249) which authorizes HHS/CDC to provide for the care and treatment of individuals detained in accordance with quarantine laws. Payment for care and treatment under this section is in the CDC’s sole discretion, subject to the availability of appropriations, and after all third-party payments have been exhausted. This section also authorizes payment for ambulance or other medical transportation services whenever the HHS/CDC considers such services to be a necessary part of an individual’s care and treatment. HHS/CDC, in consultation with state and local health departments, may make advance arrangements with medical providers through a memorandum of agreement or other mechanisms regarding payment for the care and treatment of individuals subject to public health actions.
Under this proposed section, HHS/CDC may assume responsibility for payment for the care and treatment of individuals subject to Federal apprehension, medical examination, quarantine, isolation, and conditional release. For individuals requiring hospitalization for other reasons, however, payment will not be made for costs incurred after it is determined that the individual does not have a quarantinable communicable disease because medical services beyond that point are no longer for the benefit of the public’s health. We reemphasize that any payment by HHS/CDC under this section will be made only after all third party payments have been exhausted. Through this proposal, HHS/CDC will arrange for appropriate care and treatment of individuals consistent with U.S. constitutional principles. The issuance of a formal written Federal order is also not a prerequisite for the payment of care and treatment under this section.
HHS/CDC also clarifies that it may pay for ambulance services if necessary for an individual’s care and treatment. Relocating an individual by use of ambulance services to a dedicated isolation facility can be reasonably considered to fall under “care and treatment.” It is HHS/CDC’s intent that neither medical providers, nor travelers, be financially penalized for their cooperation with public health authorities. If finalized as proposed, in implementing this section, HHS/CDC intends to coordinate with state and local health departments and medical providers. HHS/CDC specifically requests public comment on this proposed provision and whether there are any concerns regarding the proposal that all third party payments be exhausted prior to the Federal reimbursement of medical care or treatment for individuals placed under a Federal order for quarantine, isolation, or conditional surveillance.
8. § 70.14 Requirements Relating to Issuance of a Federal Order for Quarantine, Isolation, or Conditional Release
Through this rulemaking, HHS/CDC is describing the process for issuance of Federal orders for isolation, quarantine, and conditional release and required content of such public health orders. Individuals under quarantine, isolation, or conditional release, will be served with written orders describing the facts and circumstances supporting the imposition of such public health measures. This section also proposes to permit the issuance of public health orders to a group of individuals. Thus, in particular circumstances, the Federal order may be written to refer generally to a group of individuals, e.g. all individuals onboard a particular interstate flight. HHS/CDC expects that when a Federal quarantine order is written in such a manner that all individuals within that group will still receive separate copies of the group order. HHS/CDC also expects that the circumstances giving rise to a group Federal quarantine order will be exceedingly rare and that most Federal quarantine orders will be written so that they contain the names of those individuals subject to the Federal order and be issued on an individual basis. HHS/CDC specifically requests public comment on this proposed provision to issue Federal orders to entire groups rather than individuals.
This proposed provision requires that orders for quarantine, isolation, or conditional release be in writing, signed by the HHS/CDC authorizing official, and contain specific information such as the identity of the individual or group subject to the order; the factual basis for the quarantine, isolation or conditional release; and the rights and obligations of individuals subject to the order. This proposed provision also requires personal service of the order, or when such service is impracticable, that the notice be posted or published in a conspicuous location. Thus, for instance, if all individuals are to be confined in a common location, the Federal order of quarantine may be posted in a conspicuous place viewable by all of the inhabitants of that location. HHS/CDC believes that these standards for notice are consistent with due process.
HHS/CDC’s current practice is to inform individuals of its public health requirements in a language they can understand, to the extent practicable. HHS/CDC will make reasonable efforts to issue orders for quarantine, isolation, or conditional release in languages understandable to those who are subject to these orders. In circumstances where it is impractical to immediately provide a line-by-line translation of the order, HHS/CDC may take other steps to reasonably apprise individuals of the contents of the order, for example, by arranging for oral translation services or summary translations. HHS/CDC specifically requests public comment on this proposed provision and whether this provision sufficiently informs the public all of the important details concerning circumstances during which HHS/CDC would issue to groups or individuals Federal orders for quarantine, isolation, and conditional release and the duration and conditions of such orders.
9. § 70.15 Mandatory Reassessment of a Federal Order for Qarantine, Isolation, or Conditional Release
This proposed provision requires HHS/CDC to reassess the need to continue the quarantine, isolation, or conditional release of an individual or group no later than 72 hours after the Federal order was first served. A reassessment will only occur once after the first 72 hours and will not continue to reoccur every 72 hours. As part of the mandatory reassessment, HHS/CDC will review all records considered in issuing the quarantine, isolation, or conditional release order, as well as any relevant new information. If HHS/CDC decides to continue the quarantine, isolation, or conditional release or modifies it, it will notify the individual of his/her right to request a medical review. A medical review may be requested by anyone under a Federal public health order, after the mandatory reassessment is complete. As part of the mandatory reassessment and where applicable, HHS/CDC will also consider whether less restrictive alternatives would adequately serve to protect the public health. Thus, for instance, if an individual is confined in a guarded facility, HHS/CDC will consider whether less restrictive alternatives, such as home quarantine, would adequately serve to protect the public health. HHS/CDC’s review of less restrictive alternatives may include not just an analysis of the nature of the quarantinable communicable disease, but also an assessment of an individual’s willingness, ability, and likelihood of complying with less restrictive alternatives.
The mandatory reassessment is designed to minimize the chance that a quarantine, isolation, or conditional release has been misapplied and will consist primarily of a review of the written record, as well as any relevant new information. HHS/CDC has determined that 72 hours is a point at which to reassess these actions because HHS/CDC considers it the minimum amount of time needed to collect medical samples, transport those samples to laboratories, and obtain preliminary results of diagnostic testing on most quarantinable communicable disease agents. Seventy-two hours also represents an appropriate time period in which to review past actions that were taken to protect public health and to reassess the need for continued actions. HHS/CDC specifically requests public comment on this provision—in particular, whether 72 hours is the necessary amount of time to conduct a reassessment after a Federal order is first issued, or if the reassessment should take place earlier or later.
At the conclusion of the reassessment, HHS/CDC will issue a written Federal order directing that the quarantine, isolation, or conditional release be continued, modified, or rescinded. HHS/CDC may continue these actions in circumstances where it determines that such a Federal order was correctly applied and in circumstances where the existence of a quarantinable communicable disease has either been determined to be present or has not yet been ruled out.
10. § 70.16 Medical Review of a Federal Order for Quarantine, Isolation, or Conditional Release
This proposed provision provides an individual under Federal quarantine, isolation, or conditional release with an opportunity to request a medical review. HHS/CDC believes that the term “medical review” best conveys that the review is intended primarily as a medical fact-finding and is not intended to determine legal rights or duties. Upon the request of an individual under a Federal quarantine, isolation, or conditional release order, and after HHS/CDC’s mandatory reassessment of the order, HHS/CDC will, as soon as practicable, arrange for a medical review.
HHS/CDC will endeavor to convene the medical review within three to four business days of a request, but may allow for extensions, for instance, to permit the quarantined or isolated individual to confer with his/her chosen representative (or in the case of indigent individuals the appointed medical representative), review medical records, and arrange for witnesses, or when other facts and circumstances warrant. HHS/CDC believes that a more flexible standard concerning the timeframe for when a medical review must be conducted is reasonable and ensures a higher caliber of review by allowing more time to assemble and review the administrative record, conduct further examinations, and assemble necessary parties.
The medical review is for the purpose of ascertaining whether the HHS/CDC has a reasonable belief that the individual is infected with a quarantinable communicable disease, including having been exposed to the infectious agent that causes a quarantinable communicable disease, and is in the qualifying stage of the quarantinable communicable disease. The medical review is not intended to address concerns of individuals who take issue with the amenities of their confinement, but do not otherwise dispute HHS/CDC’s reasonable belief. Individuals who, for instance, object to the quality of food, housing, or entertainment available to them while subject to Federal quarantine or isolation may express such concerns through any available means, such as informally raising their concerns with the treatment facility in which they are being confined, without the need for HHS/CDC to conduct a medical fact-finding, which is the purpose of a medical review. However, as part of the medical review, the medical reviewer will consider and accept into the record evidence as to whether less restrictive alternatives would adequately serve to protect public health. Thus, for instance, if the individual is confined in a guarded facility, the medical reviewer will consider whether home quarantine would adequately serve to protect public health. HHS/CDC specifically requests public comment on this proposed provision—in particular, whether or not the public sees a role for the Federal government to ensure that basic living conditions, amenities, and standards are satisfactory when placing individuals under Federal orders.
The medical review is primarily a medical fact-finding and is also not intended to address issues of law or policy. The types of medical issues HHS/CDC expects would be raised at the medical review are those that pertain to the infectious agent at issue, the individual’s susceptibility, and the environment in which the individual may (or may not) have been exposed to the infectious agent. Individuals may also raise basic factual questions tending to refute the Director’s reasonable belief that the individual is infected with a quarantinable communicable disease, e.g., mistaken identity; not a passenger onboard an affected conveyance; not in contact with an infected individual. Individuals seeking to challenge the legal basis for their quarantine may do so through whatever legal mechanism may be available. HHS/CDC does not express an opinion regarding what form the legal action should take or what legal remedies may be available to individuals seeking to challenge their public health restrictions.
HHS/CDC will notify individuals under a Federal quarantine, isolation, or conditional release order in writing of the time and place of the medical review. HHS/CDC has defined a “medical reviewer” as a physician, nurse practitioner, or similar medical professional qualified in the diagnosis and treatment of infectious diseases who is appointed by the HHS Secretary or CDC Director to conduct a medical review. The medical reviewer may be an HHS or HHS/CDC employee, but only if the employee differs from the HHS/CDC official who issued the Federal order for quarantine, isolation, or conditional release. HHS/CDC believes that allowing for the use of HHS or HHS/CDC employees to serve as medical reviewers is consistent with standards of due process. For instance, HHS/CDC notes that it is not unusual for hospitals to rely on internal decision-makers during emergency civil commitments. The medical reviewer’s role will be to review the medical or other evidence presented, make medical or scientific findings of fact, and issue a recommendation to the CDC Director concerning whether the quarantine, isolation, or conditional release should be continued, rescinded, or modified. The medical reviewer’s role is distinct from the role of an appointed medical representative and will not be the same individual.
An individual under Federal quarantine, isolation, or conditional release may choose to be represented by anyone at their own expense during a medical review or to represent themselves. However, if an individual is indigent and cannot afford a representative, HHS/CDC will appoint a medical representative upon request at the government’s expense. HHS/CDC specifically requests public comment on this provision—in particular, whether the public believes that there may be non-indigent individuals, as defined in this NPRM, who may have difficulty affording a representative. The individual requesting such representation would be expected to sign a statement under penalty of perjury that he/she is indigent as established in the regulation. HHS/CDC would accept the signed statement as prima facie evidence that the standard for indigence has been satisfied and proceed with appointing a medical representative. HHS/CDC does not expect to independently verify income or assets at the time of the appointment. If the individual knowingly makes a false statement, then the individual could be prosecuted. The statement would include the following language, “In accordance with 28 U.S.C. 1746, I declare under penalty of perjury that the foregoing statement is true and correct.”
Because the purpose of the medical review is primarily one of medical fact-finding, it is anticipated that an appointed medical representative will be a physician or similar qualified medical professional, and not an attorney, although a patient may also choose to have an attorney present. The medical representative may be an individual from within HHS or HHS/CDC, but will be someone that is unconnected to the agency’s original decision to impose the public health restriction. HHS/CDC will use its best efforts to ensure that the medical reviewer and medical representative possess familiarity with the particular communicable disease at issue and with general principles of communicable disease transmission. The facts and circumstances of each case will dictate the type and level of expertise that may be needed in a representative. HHS/CDC believes that these procedures are consistent with the requirements for due process.
At the conclusion of the review, the medical reviewer will issue a written report to the CDC Director as to whether, in the medical reviewer’s professional judgment, the quarantine, isolation, or conditional release should be continued, modified, or rescinded. The written report will also be served on the individual under public health restrictions and his/her representative. The Director will review the written report, as well as any objections that may be submitted by the individual under public health restrictions or his/her representative contesting the medical reviewer’s findings and recommendation. Upon the conclusion of the review, the Director will promptly issue an order to continue, modify, or rescind the order.
In the event that the Director, after reviewing the medical reviewer’s report, continues or modifies the quarantine, isolation, or conditional release, the Director’s written order will include a statement that the individual may request that the CDC rescind the public health restriction, but based only on significant, new or changed facts or medical evidence showing that a genuine issue exists as to whether the individual should remain under quarantine, isolation, or conditional release. The Director’s order will not constitute final agency action until it is served on the individual or, alternatively, if individual service would be impracticable, it is posted or published. “Final agency action” means that while HHS/CDC will continue to review the need for the public health restriction to ensure that individuals are not detained longer than necessary, HHS/CDC has issued what it believes to be its final agency decision with respect to the quarantine, isolation, or conditional release.
To help facilitate the review, this section also allows HHS/CDC to issue additional or updated instructions through standard operating procedures governing the conduct of medical reviews. Such instructions, for instance, may govern the format and length of written submissions to the medical reviewer, specific number and order of witnesses, and length of oral presentations.
11. § 70.17 Administrative Records Relating to Quarantine, Isolation, or Conditional Release
This proposed provision describes the administrative record as it pertains to an individual under a Federal quarantine, isolation, or conditional release order. The administrative record is the “paper trail” that documents the agency’s decision-making process and explains the basis for the agency’s decisions. The administrative record contains the available documents that were considered by CDC in making its public health decision to quarantine, isolate, or conditionally release an individual. The administrative record will typically be compiled as documents are generated or received during the course of the agency’s decision-making, but may be compiled after the agency’s action, for example, in response to litigation.
HHS/CDC offers the following guidance concerning the administrative record. The following types of records would generally not be considered part of the administrative record: (1) Documents that are not relevant to the agency’s decision-making process, e.g., fax cover sheets, emails that do not contain relevant information or information documenting the decision-making process; (2) primary documents that did not exist or were unavailable at the time that the agency made its decision; (3) personal notes, journals, appointment calendars, and other similar documents, maintained solely for personal use and not under the agency’s control, possession, or maintenance; and (4) internal “working” drafts of documents.
Once the administrative record has been reviewed and compiled, it will be certified as the agency’s official record. The individual certifying the administrative record will be an agency official who can attest that the record is complete, accurate, and was considered by the agency in making its decision. A copy of this record will be served on the individual subject to the Federal order upon the individual’s request.
12. § 70.18 Agreements
This proposed provision allows HHS/CDC to enter into an agreement with an individual, upon such terms as HHS/CDC considers to be reasonably necessary, indicating that the individual agrees to any of the public health measures authorized under this part, including quarantine, isolation, conditional release, medical examination, hospitalization, vaccination, and treatment; provided that the individual’s agreement shall not be considered as a prerequisite to the exercise of the CDC’s authority under this part. In circumstances where an individual is unable to confirm agreement, for instance a minor or an individual with a cognitive disability or other incapacity, CDC may enter into an agreement with a parent or other appropriate guardian authorized to act on the individual’s behalf.
HHS/CDC believes that the availability of agreements is an important tool to obtain an individual’s compliance with public health measures and as a means of building trust with the individual. An agreement, for instance, may be used in circumstances where an individual agrees to comply with the instructions of public health staff, such as to not engage in travel, limit social contacts, or remain in home quarantine. An agreement will typically include a statement indicating the individual chooses to enter into the agreement on a voluntary basis, without duress or coercion, and with full knowledge of the facts and circumstances of his/her individual case. Individuals who decline to enter into such agreements will not face criminal or other penalties for not entering into such agreements. However, individuals who violate the terms of the agreement or the terms of the Federal order for quarantine, isolation, or conditional release (even if no agreement is in place between the individual and the government), he or she may be subject to criminal penalties as explained in the preamble to section 70.19. These criminal penalties will also be explained in the text of the agreement itself. HHS/CDC specifically solicits public comment on the utility and appropriateness of using agreements as described in this preamble, particularly regarding whether such agreements are confusing to individuals as they shall not be considered a prerequisite to the exercise of the CDC’s authority under this part.
13. § 70.19 Penalties
This proposed section describes the criminal penalties for violations of quarantine regulations. As prescribed in section 368 (42 U.S.C. 271) and under 18 U.S.C. 3559 and 3571(c), criminal sanctions exist for violating regulations enacted under sections 361 and 362 (42 U.S.C. 264 and § 265).18 U.S.C. 3559 defines an offense (not otherwise classified by letter grade) as a “Class A misdemeanor” if the maximum term of imprisonment is “one year or less but more than six months.” 18 U.S.C. 3571 provides that individuals found guilty of an offense may be sentenced to a fine. Specifically, an individual may be fined “not more than the greatest of”—(1) the amount specified in the law setting forth the offense; or (2) for a misdemeanor resulting in death, not more than $250,000; or (3) for a Class A misdemeanor that does not result in death, not more than $100,000. Similarly, an organization, found guilty of an offense may be fined “not more than the greatest of”—(1) the amount specified in the law setting forth the offense; or (2) for a misdemeanor resulting in a death, not more than $500,000; or (3) for a Class A misdemeanor that does not result in death, not more than $200,000. 42 U.S.C. 271 sets forth statutory penalties of up to 1 year in jail and a fine of $1,000. Therefore, it is classified as a Class A misdemeanor under 18 U.S.C. 3559. Because the alternate fines set forth under 18 U.S.C. 3571 are greater than the $1,000 set forth under 42 U.S.C. 271, and because the lower penalties established in 42 U.S.C. 271do not exempt by specific reference the offense from the applicability of the fines under 18 U.S.C. 3571 (18 U.S.C. 3571(e)), the greater penalties of 18 U.S.C. 3571(b)(5) and (c)(5) apply and will thus be incorporated into42 CFR part 70.
The intent of this proposed section is to inform individuals and entities of the available criminal penalties that currently exist in statute for violations of quarantine regulations. This section clarifies that of the statutory penalties imposed for violation of quarantine regulations (i.e.,42 U.S.C. 271 and 18 U.S.C. 3571), this rule will codify the higher penalty as established in 18 U.S.C. 3571. Furthermore, the penalties described in this section are criminal in nature referring to criminal violations of Federal quarantine regulations. Thus, these penalties would be pursued through the courts and would not be imposed administratively. HHS/CDC specifically requests public comment on this proposed provision—in particular, whether the penalties as proposed in this rule are clearly defined and the circumstances under which such penalties may be imposed.
B. Updates to Part 71
1. § 71.1 Definitions
Through this NPRM, HHS/CDC is proposing to include new and updated definitions to part 71 to provide clarity and help the public understand the intent behind the updated and new provisions.
Agreement
HHS/CDC proposes to define “agreement” in the same manner as how that term is defined under § 70.1.
Airline
HHS/CDC proposes to define “airline” in a similar manner as how that term is defined under § 70.1.
Apprehension
This provision defines apprehension in the same manner as under part 70.
Conditional Release
This proposed provision defines conditional release in the same manner as “surveillance” under § 71.1 and includes public health supervision through in-person visits by a public health official (or designee) telephone, or through any electronic or internet-based means as determined by HHS/CDC. HHS/CDC is proposing to use the term conditional release and cross-referencing the definition of surveillance so that the language of this rule is consistent with the agency’s current terminology and practices. As explained in the preamble to this definition under § 70.1, HHS/CDC is also proposing to expand this definition to permit additional forms of public health monitoring to include electronic monitoring and video chat.
Conditional Release
HHS/CDC proposes to define “conditional release” in same manner as how the term is defined under § 70.1.
Contaminated Environment
HHS/CDC proposes to define “contaminated environment” in the same manner as how that term is defined under § 70.1.
Electronic or Internet-Based Monitoring
HHS/CDC proposes to define “electronic or internet-based monitoring” in the same manner as how that term is defined under § 70.1.
Ill Person
We are proposing to update the definition of “ill person” under part 71 for a few reasons. First, we are correcting the temperature correlation from 100 degrees Fahrenheit to 100.4 Fahrenheit in the current definition so that the conversion accurately equals 38 degrees Celsius. Second, we are more closely aligning the HHS/CDC definition with the ICAO guidelines regarding illness reporting, which will also have the effect of capturing other symptoms of communicable disease of public health concern. The NPRM applies the same plain-language approach as described for the definition of “ill person” in part 70 and the above in-depth explanations and examples of the communicable diseases that such signs and symptoms might indicate also apply to this definition under part 71.
Lastly, the new proposed definition of “ill person” under part 71 includes two separate contexts and locations for the purposes of reporting the ill person: One onboard an aircraft and one onboard a vessel. Both subsections include a provision allowing HHS/CDC to include additional signs and symptoms of illness in case our understanding of the recognizable symptoms of communicable diseases of concern, such as Ebola, change or to respond to communicable diseases with unique signs and symptoms that may emerge as future concerns. Notice of such additional signs and symptoms will be published in the Federal Register.
This NPRM does not propose to create any substantive changes from current regulations in gastrointestinal illness (i.e., diarrheal) reporting for vessels, nor does it change any current operations of HHS/CDC’s Vessel Sanitation Program (VSP). HHS/CDC believes that any distinction in reporting requirements between vessels and aircrafts is justified by the fact that vessels, in particular cruise vessels, typically contain medical facilities onboard and are places where ill persons can be more easily segregated from other passengers and crew. Further, because individuals are typically onboard vessels for a longer duration than an aircraft, it is possible to track the occurrence in a 24-hour period of a greater than normal (for the person) amount of loose stools, per the existing reporting requirements under 42 CFR 71.21(b).
Indigent
This provision defines indigent in the same manner as under § 70.1. CDC specifically requests public comment on whether the use of this standard definition (150% of the applicable HHS poverty guidelines in the Federal Register) is an appropriate threshold to determine whether an individual cannot afford representation and therefore should be appointed a medical representative at the government’s expense.
Medical Examination
This provision defines medical examination in the same manner as under § 70.1.
Medical Representative
This provision defines medical representative in the same manner as under § 70.1.
Non-Invasive
While not a new concept for HHS/CDC operations, the proposed definition of non-invasive is being added to this regulation to provide the public with reasonable assurance and expectations of what measures may be employed as part of a public health risk assessment or following a report of illness. We define non-invasive as “procedures conducted by an authorized health worker or another individual with suitable training and includes the physical examination of the ear, nose, and mouth; temperature assessments using an ear, oral, cutaneous or noncontact thermometer; thermal imaging; auscultation; external palpation; external measurement of blood pressure; and other procedures not involving the puncture or incision of the skin or insertion of an instrument or foreign material into the body or a body cavity.” Non-invasive has the same meaning in part 71 as under part 70. HHS/CDC specifically requests comment concerning this definition including whether the definition aligns with common perceptions of what constitutes non-invasive procedures that may be conducted outside of a traditional clinical setting (e.g., airports, train stations).
Public Health Prevention Measures
Under section 361 of the PHS Act (42 U.S.C. 264(a)), the HHS Secretary has legal authority to approve measures to prevent the introduction, transmission, and spread of communicable disease into the United States. Furthermore, the U.S. government is generally understood to exercise plenary authority at the border. This section authorizes public health screening, risk assessment and management at ports of entry, including U.S. international airports, seaports, and land border crossings, upon terms similar to those described under part 70.
HHS/CDC believes that the provisions of this section may be applied broadly to all travelers at a U.S. port, including airports and seaports, who intend to travel internationally, regardless of whether the particular traveler is arriving into or departing from the United States. For example, it is widely known that most U.S. travelers departing the United States for purposes of engaging in international travel are doing so on round-trip itineraries and thus intend to return to the United States. Thus, it is possible for some of those travelers who may be in the incubation period of a communicable disease to return to the United States while infectious and infect others once in the United States. Collectively, over 350 million international travelers arrive into the U.S. every year. HHS/CDC’s Division of Global Migration and Quarantine (DGMQ) helps to protect our nation’s health by working to prevent the introduction and spread of communicable diseases into the U.S. While HHS/CDC has quarantine stations located at or near certain international airports and land border crossings, U.S. Customs and Border Protection (CBP) inspects international travelers arriving at U.S. ports of entry and has over 25,000 officers at all U.S. ports of entry where international travelers arrive. CBP’s unique position makes them an important partner in identifying and responding to suspected cases of communicable disease. CBP officers serve as HHS/CDC’s “eyes and ears” by visually observing travelers for certain signs of illness and notifying the HHS/CDC Quarantine Station of jurisdiction when ill travelers are detected. CDC staff are consulted to determine whether ill travelers may have a communicable disease of public health concern and whether any additional public health action is needed.
Although new to this proposed regulation, public health risk assessment and management is not a new concept. This NPRM informs the public of HHS/CDC’s authority to conduct public health risk assessment of an individual through non-invasive procedures and other means, such as observation, questioning, review of travel documents, records review, and other non-invasive means, to determine the individual’s health status and potential public health risk to others. For example, due to the 2014-2016 Ebola epidemic, HHS/CDC and DHS began enhanced entry risk assessment and management (i.e. “public health prevention measures”) at five U.S. airports (New York’s John F. Kennedy International, Washington-Dulles International, Newark Liberty International, Chicago-O’Hare International, and Atlanta Hartsfield Jackson International) to take additional steps to help prevent further spread of Ebola and to ensure that anyone found to have symptoms of Ebola at one of these airports was immediately isolated and received appropriate medical examination and care. Public health entry prevention measures enable evaluation of travelers from countries with widespread transmission of communicable disease, as well as the opportunity to provide travelers with educational materials and potential follow up. HHS/CDC requests public comment on these proposed public health prevention measures.
2. § 71.2 Penalties
This proposed provision updates the explanation of criminal penalties under 42 CFR 71.2, which currently states in existing regulation that “any person violating any provision of these regulations shall be subject to a fine of not more than $1,000 or to imprisonment for not more than 1 year, or both as provided in section 368 of the Public Health Service Act (42 U.S.C. 271).” As explained in the preamble language to the penalties provision under part 70, the intent of this section is to inform individuals and entities of the available alternate criminal penalties that currently exist for violations of quarantine regulations. This section thus codifies the alternate criminal penalties as established in 18 U.S.C. 3571.
3. 71.4 Requirements Relating to Collection, Storage, and Transmission of Airline Passenger, Crew, and Flight Information for Public Health Purposes
At present, HHS/CDC uses a multi-step process to obtain passenger contact information. HHS/CDC issues a written order under the current authority of 42 CFR 71.32(b) to the airline that requires the airline to provide HHS/CDC with contact information about the index case and passenger contacts. The order requires that the airline provide it with each traveler’s first and last name, seat number, two phone numbers and email address. Such orders can be marked “urgent” depending on the seriousness of the communicable disease. However, airlines may not be in possession of the contact information sought by HHS/CDC and may not be able to transmit contact data to HHS/CDC in a timely fashion. HHS/CDC instructs airlines to provide data when available or to inform CDC when data are unavailable.
Under this NPRM, upon confirmation by HHS/CDC of a case or suspected case of a communicable disease on board an aircraft, the operator of any airline operating a flight arriving into the United States must make certain contact information described below available within 24 hours of a request by HHS/CDC, to the extent that such data are available and already maintained by the operator. This proposed requirement is a codification of current practice, wherein CDC directly issues a manifest order to the airline, which applies to certain data elements as described in this NPRM that the airline may already have available and authorizes the airline to transmit the contact information in any format and through any system available and acceptable to both the airline and HHS/CDC. Again, because this is a proposed codification of current practices, we assume airlines will continue to submit data through current mechanisms, although we will accept others that are mutually acceptable. Further, in keeping with current practices, under this proposal, airlines are not required to verify the accuracy of the information collected, and airlines are not required to collect additional information from passengers than already collected and maintained by the carrier. Because airline manifest data are often insufficient to contact potentially exposed travelers reliably, CDC will supplement these data with information from CBP, including APIS and Passenger Name Record (PNR), consistent with current practice.
The purpose of this proposed requirement is to protect the vital health interests of passengers and crew so that individuals who have been exposed to a communicable disease during travel may be contacted, informed, and provided with appropriate public health follow-up. The measure also serves public health purposes generally by helping prevent the introduction, transmission, and spread of communicable disease into the United States. Although trends in infectious disease cannot be foreseen precisely, in recent years HHS/CDC only infrequently has had occasion to order airlines to provide the specified contact information for travelers on a given flight. Under the NPRM, orders would continue to be made on a case-by-case basis only, based exclusively on medically indicated criteria. Consistent with prior practice, such orders typically would be limited to information for certain passengers or crew who were seated within a certain distance of an individual infected or reasonably believed to be infected with a communicable disease, and are generally based on medical examination or reports from state or local health authorities. Such passengers and crew are thus at higher risk of exposure to such a disease and stand to benefit most from timely information, assessment and post exposure prophylaxis (if appropriate).
Additionally, we note also that HHS/CDC is committed to protecting the privacy of the information collected. On December 13, 2007, HHS/CDC published a notice of a new system of records (SORN) under the Privacy Act of 1974 that would be applicable to its conduct of activities under this NPRM (72 FR 70867). HHS/CDC accepted public comment on its proposed routine uses of this information at that time. As required under the Privacy Act, HHS/CDC in its notice described the proposed system of records, the proposed routine uses, disclosures of system data, the benefits and need for the routine uses of these data, our agency’s policies and procedures, restrictions on the routine uses of this information, and most importantly, our safeguards to prevent unauthorized use. Data collected from passengers; crew; ill persons; and individuals under Federal public health orders will be used to protect the vital health interests of passengers and crew so that individuals who have been exposed to a communicable disease during travel may be contacted, informed, and provided with appropriate public health follow-up. Such data will be maintained in a manner that is consistent with Article 45(2) of the International Health Regulations and will be released to authorized users only, including, where necessary, State and local government health related agencies directly involved in the contact tracing related to the original purpose of the collection. In addition, HHS/CDC will make disclosures from the system only with the consent of the subject individual, in accordance with its routine uses, or in accordance with an applicable exception under the Privacy Act or system of records notice. HHS/CDC emphasizes that the information will be maintained and used in accordance with the Privacy Act and the above-described system of records. Furthermore, HHS/CDC will apply the protections of the SORN to all travelers regardless of citizenship or nationality. HHS/CDC specifically requests public comment on this proposed provision, and has included the chart below to reflect the data elements that are collected under current practice, which CDC seeks to codify through regulation. CDC also requests comment on the applicability of the December 13, 2007 system of records (SORN) to the activities proposed in this provision (72 FR 70867), and whether the SORN sufficiently addresses the public’s concerns related to maintenance and protection of the data elements proposed. HHS/CDC requests public comment from operators of airlines regarding the request for a manifest within 24 hours and whether the provision grants sufficient time for operators to respond to manifests orders. HHS/CDC also requests comment regarding the likelihood that the passenger and crew data elements requested are already collected and maintained by airline operators for transmission to CDC.
4. § 71.5 Requirements Relating to Collection, Storage and Transmission of Vessel Passenger, Crew and Voyage Information for Public Health Purposes
Under this NPRM, upon confirmation or reasonable suspicion by HHS/CDC of a case or suspected case of a communicable disease on board a vessel, the operator of any vessel arriving into the United States must make certain contact information described below available within 24 hours of an order by the HHS/CDC, to the extent that such data are available and already maintained by the operator. This proposal is a codification of current practice and applies to any of the data elements that the vessel operator may already have available and authorizes the vessel operator to transmit the contact information in any format and through any system available and acceptable to both the vessel and HHS/CDC. Again, because this is a codification of current practices, we assume vessel operators will continue to submit data through their current mechanisms, although we will accept others that are mutually agreeable.
The purpose of this proposed requirement is to protect the vital health interests of passengers and crew so that individuals who have been exposed to a communicable disease during travel may be contacted, informed, and provided with appropriate public health follow-up. The measure also serves public health purposes generally by helping prevent the introduction, transmission, and spread of communicable disease into the United States. Although trends in infectious disease cannot be foreseen precisely, in recent years HHS/CDC only infrequently has had occasion to order vessels to provide the specified contact information. Under the NPRM, orders would continue to be made on a case-by-case basis only, based exclusively on medically indicated criteria. Consistent with prior practice, such orders typically would be limited to information for certain passengers or crew who were seated within a certain distance of an individual infected or reasonably believed to be infected with a communicable disease, and are generally based on medical examination or reports from state or local health authorities. Such passengers and crew are thus at higher risk of exposure to such a disease and stand to benefit most from timely information, assessment, and post-exposure prophylaxis (if appropriate).
The NPRM proposes the same data submission approach for vessels with minor changes to reflect the differences between air and sea travel (cabin number as opposed to seat number). The NPRM also explicitly excludes ferries, as defined under 46 U.S.C. 2101 and U.S. Coast Guard (USCG) regulations (46 CFR 2.10-25). The NPRM also excludes collecting passenger information from vessels that are carrying fewer than 13 passengers (excluding crew). HHS/CDC selected 13 passengers, excluding crew, as the dividing point since vessels with 13 or more passengers are primarily passenger vessels (as opposed to cargo vessels with ancillary passenger service) and has successfully used this criterion for many decades. HHS/CDC decided to exclude vessels with fewer than 13 passengers because of their lower expected probability of introducing and transmitting communicable disease in the U.S. HHS/CDC decided to focus public health resources on vessels with the greatest number of passengers and the greatest chance of introduction, transmission and spread of infectious disease into the United States. However, we note that we would collect contact information from these vessels if needed for an investigation. The rationale is analogous to HHS/CDC’s decision to require the collection of information of airline passengers only rather than passengers on all aircraft, where again, CDC would collect contact information if needed to protect public health.
Under the U.S. Coast Guard’s definition referenced in this NPRM, HHS/CDC is also excluding ferries that travel distances of less than 300 miles. Passengers and crew will spend much less time on these voyages as compared to a typical passenger cruise. Therefore, the opportunities for transmitting diseases are lower.
Also in keeping with current practices, under this proposal, vessel operators are not required to verify the accuracy of the information collected and HHS/CDC takes no position on what consequences the vessel operator can impose if a traveler refuses to provide the information, such as refusing to board the traveler.
Finally, we note also that HHS/CDC is committed to protecting the privacy of the information collected. On December 13, 2007, HHS/CDC published a notice of a new SORN under the Privacy Act of 1974 that would be applicable to its conduct of activities under this NPRM (72 FR 70867). HHS/CDC accepted public comment on its proposed routine uses of this information at that time. As required under the Privacy Act, HHS/CDC in its notice described the proposed system of records, the proposed routine uses, disclosures of system data, the benefits and need for the routine uses of these data, our agency’s policies and procedures, restrictions on the routine uses of this information, and most importantly, our safeguards to prevent unauthorized use. Data collected from passengers, crew, ill persons, and individuals under Federal public health orders will be used to protect the vital health interests of passengers and crew so that individuals who have been exposed to a communicable disease during travel may be contacted, informed, and provided with appropriate public health follow-up. Such data will be maintained in a manner that is consistent with Article 45(2) of the International Health Regulations and will be released to authorized users only, including, where necessary, state and local government health related agencies directly involved in the contact tracing related to the original purpose of the collection. In addition, HHS/CDC will make disclosures from the system only with the consent of the subject individual, in accordance with its routine uses, or in accordance with an applicable exception under the Privacy Act or system of records notice. HHS/CDC emphasizes that the information will be maintained and used in accordance with the Privacy Act and the above described system of records. Furthermore, HHS/CDC is committed to treating all passenger information under the SORN in the same manner regardless of citizenship or nationality. HHS/CDC requests public comment concerning the mandatory submission of crew and passenger manifests to HHS/CDC containing personally identifiable contact information for the purposes of conducting contact tracing. HHS/CDC specifically requests public comment on this proposed provision. In particular, HHS/CDC requests comment from the general public regarding whether they have any privacy concerns regarding the collection of the specified data elements proposed in this rule, the protection and maintenance of their personally identifiable information by HHS/CDC, and the disclosure of such identifiable information by the airlines and vessels to CDC during contact tracing. HHS/CDC also requests public comment from vessel operators concerning the feasibility of compliance with this provision, whether such operators anticipate having access to the proposed data elements in this rule, and if they have any concerns regarding the submission of passenger and crew information to HHS/CDC as described in this NPRM.
5. § 71.20 Public Health Prevention Measures To Detect Communicable Disease
Through this NPRM, HHS/CDC has included a proposed provision which explicitly authorizes the Director to conduct public health risk assessments of individuals or groups, at U.S. ports of entry or other locations, through non-invasive procedures as defined in 71.1 to detect the potential presence of communicable diseases. This proposal is authorized under section 361(a) of the PHS act (42 U.S.C. 264(a)) and will be implemented in a manner similar to what was described in part 70. This section also proposes to require individuals undergoing a public health risk assessment to submit information for purposes of contact tracing and assessing whether the individual may pose a communicable disease risk. HHS/CDC requests public comment concerning the proposed public health prevention measures using techniques as described in this section and the proposed scope of application of such measures at any US port of entry (such as at airports, train stations, etc.). HHS/CDC also requests public comment on the proposal to collect passenger contact tracing information during the implementation of such passenger risk assessment and management activities.
6. § 71.29 Administrative Records Relating to Quarantine, Isolation, or Conditional Release
This proposed provision explains the compiling of an administrative record regarding the issuance of Federal orders for quarantine, isolation, or conditional release. HHS/CDC will compile the administrative records in the same manner as described in the preamble language under part 70. The individual placed under a Federal public health order will be served upon request with a copy of his or her own administrative record.
5. § 71.30 Payment for Care and Treatment
This proposed provision explains the process of authorizing payment for the medical care and treatment (including room and board costs) of individuals under Federal orders for quarantine, isolation, and conditional release. HHS/CDC will implement this provision in the same manner as described in the preamble language under part 70. HHS/CDC requests public comment concerning the determination that any CDC authorization of payment for the care and treatment of individuals will be secondary to the obligation of any third-party.
6. § 71.33 Persons: Isolation and Surveillance
HHS/CDC is proposing to revise this provision to clarify that it may include other forms of public health supervision besides in-person visits or telephone reporting by the individual under a conditional release order. Such additional forms of monitoring includes “electronic or internet-based monitoring,” such as video chat and voice calls from computers, tablets and mobile devices. The proposed definition of “electronic or internet-based monitoring” is intended to be broad and would apply to any new or existing technologies that would allow for the public health supervision and monitoring of an individual under a conditional release order. For clarity, HHS/CDC is also replacing the reference to the “local health officer” with the “state or local health officer.” HHS/CDC requests public comment concerning the extension of public health observation and surveillance to include the use of electronic and internet-based technologies as defined in 71.1 for persons under a Federal conditional release order, including any privacy concerns that might arise.
7. § 71.36 Medical Examinations
This proposed provision explains the process of requiring a medical examination of arriving individuals under Federal quarantine, isolation, and conditional release. If finalized as proposed, HHS/CDC will implement this provision in the same manner as described in the preamble language under part 70. HHS/CDC requests public comment concerning the proposed activities related to medical examinations as described in this section—specifically whether medical examinations may be conducted after a Federal order for quarantine/isolation/conditional release is issued, or if medical examinations should be a prerequisite and basis of such Federal orders.
8. § 71.37 Requirements Relating to Issuance of a Federal Order for Quarantine, Isolation, or Conditional Release
This proposed provision explains the process of issuing Federal orders for quarantine, isolation, and conditional release for individuals arriving into the United States from a foreign country or foreign territory. If finalized as proposed, HHS/CDC will implement this provision in the same manner as described in the preamble language under part 70. HHS/CDC requests public comment concerning whether the information as provided in this section sufficiently informs the public of when HHS/CDC will issue a Federal order for quarantine, isolation, or conditional release, what conditions must be met for an individual to receive a Federal order, and the procedural details with which each Federal order will be implemented (e.g.,duration, scope, and enforcement).
9. § 71.38 Mandatory Reassessment of a Federal Order for Quarantine, Isolation, or Conditional Release
This proposed provision explains the mandatory reassessment of Federal orders for quarantine, isolation, and conditional release for individuals arriving into the United States. If finalized as proposed, HHS/CDC will implement this provision in the same manner as described in the preamble language under part 70. HHS/CDC requests public comment concerning whether the 72-hour limit within which a mandatory reassessment must take place represents an appropriate threshold. HHS/CDC also requests public comment on the proposed activities that mandatory reassessment would entail as specified in this section.
10. § 71.39 Medical Review of a Federal Order for Quarantine, Isolation, or Conditional Release
This proposed provision explains the process for a medical review available to arriving individuals under Federal orders of quarantine, isolation, and conditional release. If finalized as proposed, HHS/CDC will implement this provision in the same manner as described in the preamble language under part 70. HHS/CDC requests public comment concerning whether the medical review process as described in this section would adequately provide the necessary means for individuals to appeal within HHS/CDC a Federal order for quarantine, isolation, or conditional release. HHS/CDC also requests comment on the Federal appointment of a medical representative to “indigent” individuals as defined in § 71.1 and whether such a threshold would sufficiently permit individuals who cannot afford a medical representative to receive a Federally appointed medical representative.
11. § 71.40 Agreements
This proposed provision authorizes the use of agreements as explained in the preamble text explaining the use of these agreements under § 70.18. HHS/CDC specifically solicits public comment on the utility and appropriateness of using agreements as described in this preamble given that the individual’s consent shall not be considered as a prerequisite to the exercise of the CDC’s authority under this part.
12. § 71.63 Suspension of Entry of Animals, Articles, or Things From Designated Foreign Countries and Places Into the United States
This section of the NPRM proposes to implement statutory authority contained in section 362 of the Public Health Service Act (42 U.S.C. 265). This proposed provision would allow the HHS/CDC to suspend the entry of animals, articles, or things into the United States from designated foreign countries (including political subdivisions and regions thereof) or places whenever the Director determines that such an action is necessary to protect public health. If finalized as proposed, the CDC Director will designate the specific animals, articles, or things, as well as the foreign countries or places covered by the temporary prohibition on entry. The CDC Director will also designate the period of time or conditions under which the entry of imports covered by the Director’s determination into the United States will be suspended. A temporary suspension on the entry of imports covered by the Director’s determination into the United States is an important public health tool to slow the introduction of communicable disease into the United States from affected foreign countries or places.
For example, there is strong evidence to indicate that bats may be the primary host of Ebola, and HHS/CDC may wish to temporarily restrict the import of bats based on this evidence. [19] While bats are considered wildlife reservoirs of numerous zoonotic diseases (infections that can be transmitted from animals to humans), bats have been known to host deadly viral hemorrhagic fever diseases, such as Ebola.20 The risk of Ebola virus infection in bats, in particular, is not limited to any one region of the world as a recent study found serologic evidence of Ebola virus infection in bats in China.21 A 2012 study of animals (nonhuman primates, including gorillas, chimpanzees, and guenons; duiker; bats) collected during an Ebola virus disease outbreak in Africa (Democratic Republic of Congo, Gabon, Republic of Congo) determined that nearly 33% of animals found dead had laboratory evidence of Ebola virus infection.22 Although the mechanisms of transmission of Ebola virus from animal reservoirs to humans are not completely understood, at least one Ebola virus disease outbreak in Africa has been attributed to direct human contact with fruit bats. [23] African fruit bats in particular have been associated with Ebola virus infection. [24]
We note again that the ability to suspend the entry of imported animals, articles, or things is not a new practice. In the past, HHS/CDC has taken actions on an emergency basis to prevent the introduction, transmission, and spread of communicable diseases into the United States arising from affected animals, articles, or products onboard arriving conveyances. These actions have included an embargo of birds and bird products from specified Southeast Asian and other countries based on concerns arising from H5N1 influenza virus (69 FR 7165(February 13, 2004)) and an embargo of civets based on concerns arising from Severe Acute Respiratory Syndrome (69 FR 3364 (January 23, 2004)). HHS/CDC based these actions on authority contained in existing regulations in 42 CFR 71.32(b). However, unlike § 71.32(b), the new provision in this NRPM will not require that HHS/CDC demonstrate a reason to believe that a prohibited animal, article, or thing, was or will be “onboard” an arriving conveyance. HHS/CDC will exercise this new provision for the purposes of temporarily suspending the introduction of animals, articles, or things from designated foreign countries or places into the United States.
This proposed section applies broadly to any animal, article, or thing that may be brought into the United States and is not limited to items intended for commercial importation or sale. The CDC Director will designate the specific animals (by species or other taxonomic designation), articles or things as well as the foreign countries or places from which and the period of time or conditions under which HHS/CDC will suspend the entry of animals, articles, or things into the United States. For instance, the CDC Director could reinstitute the entry of imports into the United States that the CDC Director has previously prohibited when, in the CDC Director’s determination adequate measures to protect public health have been implemented in the affected foreign country or place. Under this proposal, the CDC Director may also condition the entry of imports into the United States on measures to be taken by the importer in foreign countries such as rendering a product noninfectious or, in the case of a live animal, obtaining a health certificate signed by a licensed veterinarian. HHS/CDC may also implement this authority through the issuance of specific import permits. The conditions for the permit and the application process will be published on HHS/CDC’s Web site at the time that this authority is invoked. HHS/CDC will determine the conditions of the permit on a case-by-case basis. We note that this proposed provision applies broadly to “animals, articles, or things,” and the preamble language discussing restricting imports of bats due to the risk of Ebola is simply being used as an example to highlight how this authority could be exercised. For more information on CDC’s animal import processes and procedures, please see http://www.cdc.gov/importation.
Prior to issuing a restriction on any animal, article or thing, HHS/CDC will continue to coordinate with other Federal partners with who have regulatory equities, such as USDA/APHIS, DOI/FWS, and FDA, balancing important public health issues with private property rights and effects on the global economy and foreign relations, as well as other important public interests such as the need for service animals by people with disabilities. HHS/CDC realizes there may be costs imposed on travel providers, such as vessel companies, but HHS/CDC also believes this provision is sufficiently important to global health to justify the costs. This proposed provision is meant to allow HHS/CDC to respond to events of public health concern, such as the recent outbreak of Ebola in West Africa. We note again that HHS/CDC does not anticipate a current need to exercise this authority and expects to invoke this provision rarely and based on sound epidemiological information of animal-to-human transmission either in the United States (through importation) or in a country where an outbreak is occurring, laboratory testing of humans or animals, or other evidence that suggests risk of importation of a communicable disease vector to the United States.
In implementing this section, if finalized as proposed, HHS/CDC will work with U.S. Department of Homeland Security, U.S. Customs and Border Protection (CBP) regarding any action to seize, export, or detain inbound cargo, or destruction by HHS/CDC, which CBP will then transmit to the importer and carrier of the cargo through the approved electronic data system used to file advance information or entry information for the importation of that cargo. HHS/CDC will also continue to consult with other Federal agencies that have overlapping authority, such as the Animal and Plant Health Inspection Service (APHIS) of the U.S. Department of Agriculture (USDA), the U.S. Food and Drug Administration (FDA), the U.S. Fish and Wildlife Service of the U.S. Department of Interior, and the Department of Transportation, to implement actions that may be taken with respect to prohibited cargo. HHS/CDC will also work with companies to resolve issues particular to their situation. HHS/CDC is mindful that these actions may have economic or other consequences and will only take such actions as may be necessary to protect the public health. HHS/CDC specifically requests public comment on this proposed provision, particularly regarding any concerns regarding coordination of activities with other agencies regulating the same space, as well as any industry concerns regarding whether this provision provides sufficient information detailing under what circumstances a Federal embargo on importation of animals, articles, or things would be implemented.
VII. Alternatives ConsideredBack to Top
Under Executive Order 13563 agencies are asked to consider all feasible alternatives to current practice and the rulemaking as drafted. HHS/CDC notes that the main impact of the proposals within this rule is to strengthen our regulations by codifying statutory language to describe HHS/CDC’s authority to prevent the introduction, transmission, and spread of communicable diseases. The intent of these proposed updates is to best protect U.S. public health and to inform the regulated community of these updates. One less restrictive alternative would be for HHS/CDC to stop enforcing its regulations and make compliance with current regulations voluntary. Under this scenario, HHS/CDC would not solicit contact data from airlines or provide such data to health departments in order to conduct contact investigations. HHS/CDC would not request illness and death reports on aircraft or vessels, but would still follow-up with airlines and vessel operators upon request. HHS/CDC would not prohibit interstate or international travel for persons known to be infected with quarantinable communicable diseases, or conduct entry risk assessment as was done to mitigate the potential spread of Ebola in the United States. This alternative would put travelers at greater risk of becoming infected with communicable diseases, reduce the ability of public health departments to provide post-exposure prophylaxis or other measure to prevent communicable disease spread from travelers known to have been exposed, and generally increase the risk of communicable disease transmission in the United States. Another alternative, to over-regulate by closing U.S. borders and ports of entry to incoming traffic from countries experiencing widespread transmission of quarantinable communicable diseases to protect public health is also analyzed based on the 2014-16 Ebola outbreak in West Africa. HHS/CDC is neither practicable, nor is it desirable.
Alternatives are proposed to increase or decrease HHS/CDC’s required payments for care and treatment for individuals under Federal orders as proposed in 42 CFR 70.13 and 42 CFR 71.30. Alternatives are also proposed in which HHS/CDC does not implement temporary animal import embargos (less restrictive) or does not allow importation of animals under temporary embargos for science, education, and exhibition when accompanied by a special permit.
We believe the proposed regulations described above and set forth below in text offer the best solutions for protecting U.S. public health while allowing for continued travel. HHS/CDC believes that this rulemaking complies with the spirit of the Executive Order 13563; all of these changes provide good alternatives to the current
VII. Required Regulatory AnalysesBack to Top
A. Executive Orders 12866 and 13563
HHS/CDC has examined the impacts of the proposed rule under Executive Order 12866, Regulatory Planning and Review (58 FR 51735, October 4, 1993) [25] and Executive Order 13563, Improving Regulation and Regulatory Review, (76 FR 3821, January 21, 2011). [26] Both Executive Orders direct agencies to evaluate any rule prior to promulgation to determine the regulatory impact in terms of costs and benefits to United States populations and businesses. Further, together, the two Executive Orders set the following requirements: Quantify costs and benefits where the new regulation creates a change in current practice; define qualitative costs and benefits; choose approaches that maximize net benefits; support regulations that protect public health and safety; and minimize the adverse impact of regulation. HHS/CDC has analyzed the NPRM as required by these Executive Orders and has determined that it is consistent with the principles set forth in the Executive Orders and the Regulatory Flexibility Act, [27] as amended by the Small Business Regulatory Enforcement Fairness Act (SBREFA) [28] and that, relative to the status quo, the NPRM will create minimal impact. However, there is notable uncertainty about the appropriate analytic baseline, and relative to some possible baselines, the effects of the rule are non-negligible. For example, if in the absence of the codification provided by this rule, some aspects of future CDC entry screening and risk assessment activities are found to be legally impermissible, then the status quo would not represent a reasonable approximation of the state of the world without the rule. Relative to this example baseline, the rule would lead to activities (e.g., the 2014-16 Ebola risk assessment and management program) that have both substantial costs and substantial benefits.
This regulatory impact section presents the anticipated costs and benefits that are quantified where possible. (Most of these quantified effects are relative to the status quo baseline, so unless otherwise noted, references in subsequent portions of this RIA to the “baseline” indicate the status quo.) Where quantification is not possible (as is largely the case with the non-status quo baseline), a qualitative discussion is provided of the costs and/or benefits that HHS/CDC anticipates from issuing these regulations.
Need for Rule
The 2014-2016 Ebola response highlights the inadequacies and limitations of the current traveler data collection process in which CDC must request traveler manifests from airlines and manually search for contact data in order to know who enters the United States,where they go, and how to contact them.
Airlines are often slow to respond to CDC requests for traveler manifests:
○ 30% arrive more than three days after a request,
○ 15% arrive more than six days late.
In addition, available locating information is usually incomplete: CDC receives only the name and seat number for 61% of travelers, and one or more additional pieces of information for 39% of travelers. This NPRM seeks to clarify HHS/CDC’s existing authority to request any available contact data from airlines and vessel operators to improve the timeliness and completeness of future requests.
The other change to the economic baseline that may result from this NPRM was the need to change the definition of an “ill person” to better match HHS/CDC guidance and the guidelines contained in Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation.
In addition, HHS/CDC believes that there is a need to better communicate to the public the actions that it has taken in accordance with its regulatory authority under 42 CFR 70.6 Apprehension and detention of persons with specific diseases, 42 CFR 71.32 Persons, carriers, and things, and § 71.33—Persons: Isolation and surveillance. HHS/CDC believes it is necessary for the public to better understand actions that may be taken to prevent the importation of communicable diseases and to elucidate the due process of individuals under Federal orders for isolation, quarantine, or conditional release. HHS/CDC also believes it is important to elucidate when CDC may authorize payment for the care and treatment of individuals subject to medical examination, quarantine, isolation and conditional release.
Finally, HHS/CDC believes it is important to elucidate its regulatory authority to suspend entry of animals, articles or things from designated foreign countries and places into the United States when importation increases the risk of the introduction and/or transmission of a communicable disease within the United States.
The specific market failure addressed by these regulations is that the costs associated with the spread of communicable diseases impacts the entire U.S. population, not just the group of persons currently infected with communicable diseases or with business interests in providing interstate or international travel to persons or animals infected with communicable diseases.
The economic impact analysis of this NPRM is subdivided into four sections:
1. An analysis of proposed 42 CFR 70.1, 42 CFR 71.1/71.4/71.5, for which the primary costs may be incurred by aircraft and vessel operators and the primary benefit is improved public health responsiveness to assess and provide post-exposure prophylaxis to travelers exposed to communicable diseases of public health concern.
2. An analysis of a number of provisions that aim to improve transparency of how HHS/CDC uses regulatory authorities to protect public health. These changes are not intended to provide HHS/CDC with new regulatory authorities, but rather to clarify the agency’s standard operating procedures and policies, and due process rights for individuals. HHS/CDC believes that such clarity is an important qualitative benefit of the provisions proposed this NPRM, but is not able to monetize this increase in clarity in a robust way. The costs and benefits associated with the 2014-2016 Ebola enhanced risk assessment and management program are used to illustrate the costs and benefits of implementation of some of these authorities, and are especially relevant when analyzing the effects of the rule relative to a non-status quo baseline.
3. An analysis of the proposed revisions to 42 CFR 70.13/71.30: Payment for care and treatment, which are not expected to lead to a change in HHS/CDC policy under which HHS/CDC may act as the payer of last resort for individuals subject to medical examination, quarantine, isolation, and conditional release under Federal orders. The primary benefit of codification is increased transparency around HHS/CDC policies to assist in paying for treatment or transportation for individuals under Federal orders. The analysis for these provisions is an examination in potential transfer payments between HHS/CDC and healthcare facilities that provide treatment to individuals under Federal orders or to other payers.
4. An analysis of the proposed 42 CFR 71.63: Suspension of entry of animals, articles, or things from designated foreign countries and places into the United States. In this NPRM, HHS/CDC is elucidating its existing regulatory authority. HHS/CDC cannot predict how often such authority may be used in the future or for what purpose. HHS/CDC previously exercised this authority on June 11, 2003, “when under 42 CFR 71.32(b), HHS/CDC implemented an immediate embargo on the importation of all rodents from Africa (order Rodentia).” [29] A simple economic impact analysis of this embargo is performed to demonstrate the costs and benefits of one example, but HHS/CDC does not anticipate an increase in frequency of such actions based on the provisions included in this NPRM. The primary purpose of the analysis is to demonstrate potential costs and benefits using a realistic example.
Each of the four analyses has a unique set of costs and benefits so four separate analyses are performed as summarized below.
Cost Overview Proposed 42 CFR 70.1, 42 CFR 71.1/71.4/71.5, Using a Status Quo Baseline
The quantified costs and benefits of the Notice of Proposed Rulemaking are estimated for the following stakeholders: Air and maritime conveyance operators, state and local public health departments (Ph.D.s), individuals exposed to communicable diseases during travel and United States Government (USG). The most likely estimates of primary costs are low ($35,785, range $10,959 to $65,644) because the NPRM primarily codifies existing practice or improves alignment between regulatory text and the symptoms reporting guidelines provided by ICAO. The cost estimates are based on an increase in
- the number of illness reports delivered by airlines and vessel operators, relay of air illness reports by the Federal Aviation Authority through air traffic control, processed by HHS/CDC;
- increased costs for airlines and vessel operators to comply with HHS/CDC requests for traveler contact data;
- increased costs for state and local public health departments to follow up with a larger number of travelers exposed to communicable diseases during travel.
Benefits, Using a Status Quo Baseline
The best estimate of quantified benefits of the NPRM is also relatively small $117,376 (range $26,337 to $312,054) and mostly results from increased efficiencies for HHS/CDC and state and local public health departments to conduct contact investigations among travelers on aircraft and vessels exposed to communicable diseases and reduced costs associated with measles and tuberculosis morbidity and mortality in exposed travelers.
Other potential but non-quantified benefits of the NPRM would be associated with future outbreaks of infectious disease cases for which improved compliance by airlines and vessel operators to provide available traveler contact data would reduce onward spread of disease in the destination communities of exposed travelers. In addition, the change to the definition of “ill person” may also increase reporting of communicable diseases of public health concern onboard conveyances. Reduction in onward spread would also lead to the ability of the public health establishment to reduce effects of disease outbreaks, e.g., delay the spread of disease until a vaccine is available orlimit the numbers of outbreaks and cases or reduce public anxiety associated with the risk of transmission. There may also be a reduction in the economic costs of many business sectors such as avoidance of costs to the travel and tourism industry 30 31 when a disease is contained in its early stages.
Section 202(a) of the Unfunded Mandates Reform Act of 1995 requires that agencies prepare a written statement, which includes an assessment of anticipated costs and benefits, before proposing “any rule that includes any Federal mandate that may result in the expenditure by State, local, and tribal governments, in the aggregate, or by the private sector, of [$$146,000,000, in 2015 USD] or more.” Not only will this NPRM not cost State, local and tribal governments any expenditure, it is probable that these stakeholders who might be engaged in contact tracing may see a reduction in costs if the proposed NPRM is implemented and there is an improvement in airline compliance with HHS/CDC requests to provide traveler data.
The Notice of Proposed Rulemaking
Traveler contact information will only be requested by HHS/CDC after a case of serious communicable disease (index case) is reported in a person who traveled on a commercial airline while contagious. Examples of serious communicable diseases include measles, novel influenzas, and viral hemorrhagic fevers such as Ebola among others. This type of situation necessitates identifying and locating passengers seated near the index case in order to conduct a contact investigation (CI). This NPRM would lead to better health outcomes if public health departments are more quickly and effectively able to contact persons potentially exposed to the index case on an aircraft or vessel. These increased efficiencies should lead to smaller infectious disease outbreaks and fewer public health resources needed to control an outbreak.
There are multiple communicable diseases (e.g., measles, tuberculosis, and Ebola) that may necessitate a contact investigation to prevent spread of disease in the community. HHS/CDC was unable to quantify the benefits of preventing the spread of all diseases as a group because of differences in the characteristics of each disease. The differences with respect to potential spread and impact make it difficult to assess the benefits that may accrue from reduced spread of all diseases. The quantified analysis focuses on the two diseases that generate the greatest number of contacts to follow up: Measles and tuberculosis.
The ongoing persistence of measles in the United States provides a good example of the need for this NPRM. In 2000, measles was declared no longer endemic in the United States due to high vaccination rates. Cases and outbreaks of measles continue to occur, however, as a result of importation from other countries and lack of adherence to the recommendation for measles vaccination (http://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/mmr.html). The United States is currently discovering the greatest number of measles cases that have been identified since the declaration of measles elimination; 97% of recent cases were associated with importations from other countries. Of 45 direct importations, 40 occurred in U.S. citizens after traveling abroad. [32]
Among air travelers exposed to measles during flights, post-exposure prophylaxis (PEP) with measles-containing vaccine (within 72 hours) or immune globulin (within 6 days) can prevent onset of disease, [33]halting outbreaks before they begin. However, without accurate and timely contact data, it is frequently difficult to intervene within these timelines. A recent analysis showed that 9 cases likely occurred as a result of exposure during 108 flights with 74 case-travelers over 3 years. Although there was no onward transmission from these 9 cases, [34]future cases may lead to larger outbreaks.
Measles outbreaks can have substantial associated costs. One study showed that 16 outbreaks with 107 confirmed measles cases cost an estimated $2.7 million to $5.3 million U.S. dollars for public health departments to contain. [35] This corresponds to an average cost per outbreak of about $250,000 in 2015 USD. In comparison, a total of 125 cases occurring in 8 states and three countries were associated with a single measles outbreak that originated in late December 2014 in amusement theme parks in Orange County, California. [36] Thus, the number of cases in this one outbreak exceeded the total number of outbreak-associated cases identified in 16 outbreaks during 2011. The source of the initial exposure has not been identified so it is not possible to determine where this index case was exposed. However, this example demonstrates the speed with which communicable diseases can be transmitted and the importance of quickly identifying persons that may have been exposed during air or maritime travel. It is possible that the costs of this one outbreak, which spread across 8 states, exceeded the total costs of all 16 outbreaks that occurred in 2011 and were estimated to cost public health departments a total of $2.7 million to $5.4 million dollars. [37]
In the absence of interventions by public health departments, travelers infected with measles during international travel would be as likely as any other individuals to initiate a measles outbreak. In the absence of HHS/CDC efforts to retrieve and transmit contact data, public health departments would not be able contact travelers to provide post-exposure prophylaxis and to self-monitor for potential measles symptoms.
Summary of Quantifiable and Qualitative Results of the Regulatory Impact Analysis
The Summary Table provides estimated total monetary results for stakeholders’ costs and benefits of implementing the NPRM. HHS/CDC finds (Summary Table) that the lower bound estimates of quantified costs and benefits are zero because this NPRM is primarily codifying existing guidance and practice. The Summary Table includes estimates associated with changes to the definition of `ill person’ in 42 CFR 70.1/71.1 and the codification of international traveler data collection processes of aircraft and vessel contact investigations under42 CFR 71.4/71.5. The best estimates of annual costs are $35,785 compared to the best estimate of annual benefits at $117,376. The upper bound annual quantified costs are $65,644 and the upper bound quantified benefits are $312,054. Lower bound quantified costs are $10,959 and benefits are $26,337.
The measles and tuberculosis examples should not be considered a complete estimate of non-quantified benefits associated with this NPRM, because the impact of this NPRM to mitigate many different types of infectious disease outbreaks cannot be quantified. It just provides examples based on the two diseases for which contact investigations are most frequently undertaken. Besides communicable diseases commonly reported in the United States (e.g., measles, tuberculosis), this NPRM may also improve HHS/CDC’s ability to respond to diseases that are infrequently diagnosed in the United States (e.g., Ebola, novel influenza, Middle East Respiratory Syndrome). For example, it is possible that HHS/CDC may need to prepare to address both Ebola and another disease such as novel influenza or Middle East Respiratory Syndrome (MERS) occurring in two separate countries or regions during a given year. For example, in 2014, two international travelers on commercial flights from the Middle East arrived in the United States while infected with MERS and two international travelers on commercial flights from West Africa arrived while infected with Ebola. Regardless of the infectious disease scenarios faced by HHS/CDC in a given year, this NPRM will improve HHS/CDC’s ability to mitigate infectious diseases in the future. To the extent that the NPRM would lead to improved responsiveness of airlines and vessel operators to HHS/CDC traveler data requests, HHS/CDC may become better able to respond to infectious diseases threats and (1) reduce case-loads during infectious disease outbreaks, (2) reduce public anxiety during disease outbreaks, (3) mitigate economic impacts on businesses as a consequence of reduced public anxiety, and 4) reduce the amount of personnel labor time to conduct large-scale contact investigations in response to a new infectious disease or one with serious public health and medical consequences like Ebola .
| Category | Most likely estimate | Lower bound estimate | Upper bound estimate | Source citation (RIA, preamble, etc.) |
|---|---|---|---|---|
| ** Costs and benefits relative to a non-status quo baseline would be of much greater magnitude than the estimates shown in this table. | ||||
| Benefits | ||||
| Annual monetized benefits (0% discount rate) | $117,376 | $26,337 | $312,054 | RIA. |
| Qualitative (unquantified benefits) | To the extent that improved responsiveness of airlines and vessel operators to HHS/CDC traveler data requests results from the implementation of the provisions proposed in this NPRM, HHS/CDC may become better able to respond to infectious diseases threats and (1) reduce case-loads during infectious disease outbreaks, (2) reduce public anxiety during disease outbreaks, (3) mitigate economic impacts on businesses as a consequence of reduced public anxiety, and (4) reduce the amount of personnel labor time to conduct large-scale CIs in response to a new infectious disease or one with serious public health and medical consequences like Ebola. | RIA. | ||
| Costs | ||||
| Annual monetized costs (0% discount rate) | $35,785 | $10,959 | $65,644 | RIA. |
| Annual quantified, but unmonetized, costs | None | RIA. | ||
| Qualitative (unquantified) costs | None | RIA. | ||
Regulated Entities: Airlines and Vessel Operators
The group of entities that may be affected by this NPRM would include international and interstate aircraft operators, vessel operators, travelers, state or local health departments and the Federal government agencies that interact with these groups. Since this NPRM primarily updates regulatory requirements to better match current practice, the economic impacts are marginal changes to current practice that result from codification of current practices.
The North American Industry Classification System (NAICS) is used by Federal statistical agencies in classifying business establishments for the purpose of collecting, analyzing, and publishing statistical data related to the U.S. business economy. A summary of the total numbers of each entity is summarized in Table 3.
| NAICS codes | NAICS description | Number of firms in industry |
|---|---|---|
| 481111 | Scheduled Passenger Air Transportation | 264 |
| 481112 | Scheduled Freight Air Transportation | 212 |
| 481219 | Other Nonscheduled Air Transportation | 516 |
| 483111 | Deep Sea Freight Transportation | 191 |
| 483112 | Deep Sea Passenger Transportation | 54 |
| 483113 | Coastal and Great Lakes Freight Transportation | 337 |
| 483114 | Coastal and Great Lakes Passenger Transportation | 110 |
| 483211 | Inland Water Freight Transportation | 318 |
| 483212 | Inland Water Passenger Transportation | 193 |
Statistics of U.S. Businesses, 2013 U.S. all industries. [38]
2012 North American Industry Classification System (NAICS). [39]
According to a report by the Federal Aviation Administration, in 2012, U.S. civil aviation-related economic activity generated $1.5 trillion and supported 11.8 million jobs with $459.4 billion in earnings. [40] In 2015, the domestic U.S. market for air travel included 696 million passengers and the international market included another 198 million travelers. [41]
In 2011, there were approximately 11 million North American cruise ship passengers spending 71.8 million passenger nights on board vessels. The cruise ship market was highly concentrated with four firms accounting for 98% of the total market. [42] In total, approximately 18 million travelers enter the United States each year via cruise or cargo ships. [43]
The domestic/international air carrier market is an ever-shifting corporate landscape. Both U.S. and foreign airlines engage in ”code-sharing” arrangements, whereby the marketing carrier places its call sign (or code) on the operating carrier’s flight. For purposes of this rule, reporting duty would require the operating carrier to report on allpassengers and crewmembers, whether traveling on the operator’s code or another carrier’s.
The complexity of the domestic/foreign airline-corporations’ legal and financial arrangements makes it very difficult to ascertain exactly how each and every domestic and foreign airline would be affected by the implementation costs associated with this NPRM; presumably, some of the costs might be passed along to the carrier putting its code on the operating carrier, pursuant to the particular terms of each applicable contract.
Under this NPRM, the operator of any airline operating a flight arriving into the United States must make certain contact information described below available within 24 hours of a request by HHS/CDC, to the extent that such data are available to the operator. This requirement also applies to the operator of any vessel carrying 13 or more passengers (excluding crew) and, which is not a ferry as defined in under 46 U.S.C. 2101 and U.S. Coast Guard (USCG) regulations (46 CFR 2.10-25). This proposed requirement is a codification of current practice, and applies to any of the data elements that the airline or vessel operator may have available and authorizes the airline or vessel operator to transmit the contact information in any format and through any system available and acceptable to both the airline and HHS/CDC. Again, because this is a proposed codification of current practices, HHS/CDC assumes airlines and vessel operators will continue to submit data through current mechanisms, although HHS/CDC will accept others that are mutually acceptable.
In keeping with current practices, under this proposal, airlines and vessel operators are not required to verify the accuracy of the information collected and HHS/CDC takes no position on what consequences the airlines or vessel operators can impose if a traveler refuses to provide the contact information, such as refusing to board the traveler. To simplify the analysis and to develop conservative cost estimates, HHS/CDC assumed that all costs to airlines and vessel operators would be passed along to U.S.-based airlines, vessel operators, or U.S. consumers.
Diseases Affected by the Rule
HHS/CDC has gathered statistics, or reported information on, a number of notifiable and quarantinable diseases (Table 4) that form the basis for estimates of quantitative and qualitative benefits.
| Measles | Pertussis |
| Tuberculosis | Rubella. |
| Rabies | Viral Hemorrhagic Fevers. |
| Meningococcal disease | Middle East Respiratory Syndrome Coronovirus (MERS). |
| Varicella |
These diseases fall into two classes. The first class is the group of diseases that HHS/CDC currently encounters with some frequency (routine diseases): Tuberculosis, measles, meningococcal disease, pertussis and rubella. The second class is a group of new or emerging diseases, or diseases with serious public health and medical consequences, that are not currently prevalent, but are foreseeable as a future threat, e.g., severe acute respiratory syndromes (including SARS and MERS), pandemic influenza, Ebola.
Contact Investigations and Diseases—Interstate and International
The number of travelers exposed to an index case that are subject to a contact investigation (CI) varies by disease and may include only the two passengers sitting adjacent to the index case (meningococcal disease or pertussis) or as much as the entire aircraft (e.g., initial investigations of cases of MERS or Ebola) (Table 5). The entire aircraft or vessel may be subject to CI if the disease is new and transmission patterns are not well understood (e.g., MERS) or if the disease is felt to have serious medical or public health consequences (e.g., Ebola). Some CIs are only initiated for long-duration travel (e.g., tuberculosis for flights of 8 hours or longer). For other diseases (e.g., measles, MERS), CIs are undertaken regardless of duration.
The table also includes criteria to be considered a contact for persons exposed on vessels. In contrast to air contact investigations, most maritime contact investigations are undertaken before travelers disembark from vessels. Another difference between air and maritime contact investigations is that varicella contact investigations are frequently undertaken among maritime travelers on vessels, but are not pursued for air travelers. In addition, HHS/CDC has not yet had to conduct a contact investigation for Middle East Respiratory Syndrome or viral hemorrhagic fever for travelers exposed on vessels.
| Disease | CI Initiated if | Persons contacted, aircraft | Persons contacted, vessels | Recommended activities |
|---|---|---|---|---|
| Ebola | All cases | All passengers and crew as of April 2016. In the future, the recommendation may change to include fewer passengers and crew | Cruise vessel—any passenger or crew who made have come into contact with the index case’s body fluids while the index case was symptomatic Cargo vessel—all on board the vessel while the index case was symptomatic | Monitoring for 21 days after last potential exposure. |
| Measles | All cases if notification received within 21 days of flight | Passengers seated within 2 rows either direction of the index case, all babies-in-arms, crew in same cabin All passengers and crew on flights with <50 seats | Direct face-to-face contact or shared confined space >1 hour with symptomatic case-patient | MMR vaccination if unvaccinated and <72 hrs since exposure; immune globulin if indicated and within 6 days of exposure. |
| Meningococcal disease | Case meets the definition of meningococcal disease within 14 days of travel For air travel: flight >8 hrs (or shorter flights if direct exposure reported) | Passengers or crew sitting directly to the left and right of the index case or with potential for direct contact with oral or respiratory secretions | Cruise vessels—Cabin mates of or potential for direct contact with oral or respiratory secretions of case-patient during the 7 days prior to symptom onset until 24 hours after implementation of effective antimicrobial therapy Cargo vessels—All on board the vessel during the 7 days prior to symptom onset of case-patient until 24 hours after implementation of effective antimicrobial therapy | Post-exposure chemoprophylaxis. |
| New or reemerging influenza viruses | All cases during early stages of international spread | All passengers and crew | All crew and passengers | Monitoring for 10 days after last potential exposure; possible serologic testing. |
| Pertussis | All cases if notification is received within 21 days of travel | Passengers sitting next to index case | Direct face-to-face contact or shared confined space >1 hour with symptomatic case-patient | Post-exposure chemoprophylaxis. |
| Rubella | All cases if notification is received within 60 days of travel | Passengers seated within 2 rows + crew in same cabin All passengers and crew on flights with <50 seats | Direct face-to-face contact or shared confined space >1 hour with symptomatic case-patient | Serologic testing and guidance for pregnant women. |
| Severe Acute Respiratory Syndromes | All cases | SARS-Coronavirus: All passengers and crew MERS: All passengers and crew contacted during 2014 CIs. Future CIs will include passengers seated within 2 rows of index case | Cruise vessel—any passenger or crew who had direct face-to-face contact or shared confined space >1 hour with symptomatic case-patient Cargo vessel—all on board the vessel while the index case was symptomatic | Monitoring for 10-14 days after last potential exposure; potential serologic testing. |
| TB | Notification received within 3 months of travel, clinical criteria met For air travel: Flight >8 hrs | Passengers seated within 2 rows | Cargo vessel: All crew members within 3 months of diagnosis who worked with case-patient Cruise vessel: Passenger travel companions or crew working in close proximity/sharing living quarters | Aircraft: Testing for latent TB infection; chest radiograph if the LTBI test is positive Vessels: Clinical assessment for symptoms and chest radiograph. |
| Varicella | All cases on vessels | NA | Any person who has had ≥5 minutes of direct face-to-face contact with a varicella case during the infectious period | Varicella vaccination if unvaccinated/non-immune and <3 days since exposure (possibly up to 5 days) High-risk contacts evaluated Varicella Zoster immune globulin if <10 days after exposure. |
The Quarantine Activity Reporting System (QARS), which contains, among other data, information collected under OMB Control Numbers0920-0134, 0920-0488, 0920-0821, and 0920-0900, is a web-based and secure electronic system that supports collection of data for ill persons on inbound or interstate flights and vessels and at land border crossings; infectious disease threats, and follow-up actions. Currently, CDC Quarantine Stations at U.S. ports of entry are using the system to record their daily activities. All CIs undertaken by HHS/CDC are documented in QARS.
CIs for international flights from January 2010 through December 2015 are summarized in Table 6. More than half (73.2%) were initiated as a result of tuberculosis cases. Measles is the next most common disease (20.8%). The remaining 6% are subdivided across rubella, pertussis, meningococcal disease and other diseases. This table also includes CIs undertaken for MERS.
| Disease | Total investigations | Total contacts | Average investigations per year | Average contacts per year | Percent of total contacts |
|---|---|---|---|---|---|
| [QARS Data] a | |||||
| a In May 2011, CIs were discontinued for international outbound flights. To give a better picture of what CIs will look like under this new protocol, flights from January 2010 to May 2011 have been excluded from the above-reported counts. In addition, CIs for mumps have been discontinued. Prior to discontinuation, there were approximately 25 contacts per year investigated for mumps. | |||||
| b For these CIs, contact information for the entire flight was required. | |||||
| In rare instances, a disease is ruled out after a CI has happened. | |||||
| Influenza, avian | 0 | 0 | 0.0 | 0.0 | 0.0 |
| MERS Coronavirus b | 2 | 270 | 0.3 | 45.0 | 1.7 |
| Measles | 94 | 3,381 | 15.7 | 563.5 | 20.8 |
| Meningococcal disease | 8 | 9 | 1.3 | 1.5 | 0.1 |
| Other | 3 | 97 | 0.5 | 16.2 | 0.6 |
| Pertussis | 11 | 18 | 1.8 | 3.0 | 0.1 |
| Rabies | 3 | 4 | 0.5 | 0.7 | 0.0 |
| Rubella | 17 | 532 | 2.8 | 88.7 | 3.3 |
| TB (clinically active) | 318 | 11,928 | 53.0 | 1988.0 | 73.2 |
| Viral hemorrhagic fever | 7 | 53 | 1.2 | 8.8 | 0.3 |
| Total | 463 | 16,292 | 77.2 | 2,715 | |
HHS/CDC also requests traveler contact data to support contact investigations for travelers exposed to infectious diseases on interstate flights. The numbers of investigations and contacts during 2010-15 are summarized in Table 7. In contrast to international flights, very few contact investigations for tuberculosis were undertaken on interstate flights, because most interstate flights do not meet the 8-hour time requirement for tuberculosis contact investigations (Table 5). The majority of contacts were investigated after exposure to measles cases (76%) followed by MERS(8.4%) and viral hemorrhagic fevers including Ebola (8.0%).
| Disease | Total investigations | Total contacts | Average number of investigations per year | Average number of contacts per year | Percent of total contacts |
|---|---|---|---|---|---|
| [QARS Data] | |||||
| Note: | |||||
| a For these CIs, contact information for the entire flight was required. In rare instances, a disease is ruled out after a CI has happened. | |||||
| Measles | 72 | 3,033 | 12.0 | 505.5 | 76.1 |
| Meningococcal disease | 1 | 1 | 0.2 | 0.2 | 0.0 |
| MERS Coronavirus a | 2 | 334 | 0.3 | 55.7 | 8.4 |
| Other | 0 | 0 | 0.0 | 0.0 | 0.0 |
| Pertussis | 43 | 83 | 7.2 | 13.8 | 2.1 |
| Rabies | 3 | 3 | 0.5 | 0.5 | 0.1 |
| Rubella | 8 | 172 | 1.3 | 28.7 | 4.3 |
| TB (clinically active) | 2 | 40 | 0.3 | 6.7 | 1.0 |
| Viral hemorrhagic fever | 4 | 319 | 0.7 | 53.2 | 8.0 |
| Total | 135 | 3,985 | 22.5 | 664.2 | |
The numbers of contacts for maritime contact investigations are summarized in Table 8. For maritime investigations, the majority of contacts were investigated for varicella (~79%) followed by tuberculosis (~13%) and measles (~6%). Most of the varicella and measles contact investigations were initiated while travelers were still on vessels. Besides the investigations listed in Table 8, gastrointestinal illness cases on cruise vessels carrying 13 or more passengers are reported to HHS/CDC’s Vessel Sanitation Program and cases of Legionnaires’ disease are reported directly to CDC’s Respiratory Diseases Branch.
| Passengers per voyage | Total investigations | Total contacts | Average number of investigations per year | Average number of contacts per year | Percent of total contacts |
|---|---|---|---|---|---|
| [January 2010-December 2015] | |||||
| a One CI for varicella involved entire crew of the vessel (1224). | |||||
| Measles | 5 | 288 | 0.83 | 48 | 6.3 |
| Meningococcal disease | 3 | 22 | 0.5 | 3.67 | 0.5 |
| MERS Coronavirus ** | 0 | 0 | 0 | 0 | 0.0 |
| Other | 1 | 9 | 0.17 | 1.5 | 0.2 |
| Pertussis | 3 | 14 | 0.5 | 2.33 | 0.3 |
| Rabies | 0 | 0 | 0 | 0 | 0.0 |
| Rubella | 2 | 26 | 0.33 | 4.33 | 0.6 |
| TB (clinically active) | 50 | 585 | 8.3 | 97.5 | 12.8 |
| Viral hemorrhagic fever | 0 | 0 | 0 | 0 | 0.0 |
| Varicella (chickenpox) a | 206 | 3,627 | 34.3 | 604.5 | 79.3 |
| Total | 270 | 4,571 | 45 | 761.8 | 100.0 |
Traveler Contact Data Requests From Airlines
For routine contact investigations performed during business hours without HHS/CDC surge staff, HHS/CDC experience suggests that following a flight, it takes airlines up to seven days to respond to a single request for traveler manifest and contact data information currently collected.
Contact tracing is most effective at reducing cases of communicable disease at the early stages of a potential outbreak as soon after initial exposure as possible. Therefore, if an efficient contact system is not in place when the first ill travelers arrive, the benefits of contact tracing are greatly diminished.
Contact data requests only occur after a case of serious communicable disease (index case) is reported in a person who traveled on a commercial airline or vessel while contagious. This type of situation necessitates identifying and locating travelers seated near the index case in order to conduct a CI.
At present, HHS/CDC uses a multi-step process to obtain traveler contact information from airlines. HHS/CDC issues a written order to the airline that requires the airline to provide HHS/CDC with contact information about the index case and traveler contacts. The order cites current regulatory language in 42 CFR 71.32(b), as authorized by 42 U.S.C. 264. HHS/CDC requests that the airline provide it with the traveler’s first and last name, seat number, two phone numbers and email address. HHS/CDC instructs airlines and vessel operators to provide data when available or to report when data are unavailable. The time it takes for HHS/CDC to obtain the traveler contact data can range from a few hours to a few days. From 2010 through May 2015, about 70% of manifests from airlines arrived within 3 days of the request, 15% arrived between 3 and 6 days after a request, 15% arrived after more than six days, and nine requests took more than a month or were never received by HHS/CDC.
At present, HHS/CDC requests that airlines and vessels provide available traveler contact data within 24 hours for “urgent” manifest requests. In current practice, requests for contact data are only considered “non-urgent” for contact investigations in which travelers had rubella (for which there is no available prophylaxis) or tuberculosis or for situations in which CDC is not notified of travelers diagnosed with some communicable diseases until after a certain amount of time during which prophylaxis would be effective (e.g., for measles: 6 days). If the analysis is limited to diseases where requests for traveler contact data are marked “urgent” by HHS/CDC (measles, meningococcal disease, MERS, viral hemorrhagic fevers, and rabies), performance improved such that 51% arrived within 24 hours of a request, 33% arrived between 1-3 days after a request, 13% between 3-6 days and only 3% arrived after 6 days.
While HHS/CDC requires that all information be provided upon first order for information, HHS/CDC has consistently seen that the information provided by a majority of airlines appears limited to frequent flyer information, or other limited contact information. Overall, the completeness of data provided by airlines varied such that airlines generally fell into two categories. Some airlines always provided only the passenger name and seat number. Other airlines would provide some additional contact information for passengers. However, even among these airlines, contact data for some of the passengers only included names and seat numbers. Considering all requests from 2014, at least one additional piece of contact information was provided for only about 39% of passengers. If the sample were restricted to only flights for which any contact information was provided (1,270 out of 2,411 total passengers), the fraction of passengers with at least one piece of contact information beyond name and seat number increased from 39% to 73.9%. This contact information would include U.S. address for 41.7% of passengers and one phone number for 45% of passengers. As a result of HHS/CDC’s use of available information and technology and its partnerships with other Federal agencies, contact tracing of exposed travelers can now be accomplished more rapidly than would be possible if only the contact data provided by airlines were used.
Since the proposed NPRM does not change the timeframe or amount of data requested from airlines or vessel operators, the most likely economic impact is a small change in the amount of effort for airlines to provide more complete and timely information. To the extent that airlines would become more compliant, it would require some airline information technology staff to expedite requests or to search in more depth for available data. HHS/CDC estimates this may require one hour of staff time per request. HHS/CDC has no way to predict how much more complete, timely, or accurate contact from airlines would become as a result of this NPRM. On average, HHS/CDC acted upon 77 requests per year to airlines for international traveler contact data between 2010 and 2015 (Table 6). In addition, HHS/CDC made 22.5 requests per year for interstate traveler data (Table 7) over the same period. There were 45 contact investigations per year among travelers on vessels (Table 8); however, most of these were undertaken before travelers disembarked vessels in which case contact data could be collected directly from exposed travelers as part of the investigation. The number of maritime contact investigations requiring manifest requests after disembarkation is estimated to be less than 10 per year.
Overall, including international air, interstate air, and maritime activities, the estimated number of contact data requests after disembarkation was rounded up to 125 to account for the fact that HHS/CDC sometimes requests traveler contact data for infectious disease events prior to confirmed diagnoses. On occasion, it turns out that travelers are not infected with diseases that require a public health response. This rounding up should also account for a year in which there is a significant increase in the number of contact investigations among exposed air or maritime travelers.
The average wages for computer and information systems managers (occupation code 11-3021) reported in the Bureau of Labor Statistics, May 2015 Occupational Employment Statistics [44] were $63.27 per hour. On average, under the baseline, HHS/CDC assumes that it would require 6 hours of work by airlines to search databases and provide data. For the NPRM, HHS/CDC assumes that a management-level computer specialist will spend additional time to provide the best possible contact data for potentially exposed travelers. The base salary is multiplied by an overhead multiplier of 100% to account for non-wage benefits and other overhead costs for supporting each employee (Table 9). The lower bound estimate is no change from current practice, while the upper bound estimate assumes 2 hours of time instead of one. HHS/CDC specifically solicits public comment on cost estimates associated with improved provision of travel contact data by affected airlines and vessel operators.
| Average number of manifest requests per year | Increased effort to provide more complete or more timely passenger contact data (hrs) | Average hourly wage rate of IT staff (2015 USD) | Overhead multiplier (percent) | Total cost | |
|---|---|---|---|---|---|
| Baseline | 125 | 6 | $63.27 | 100 | $94,905 |
| Best estimate | 125 | 1 | 63.27 | 100 | 15,818 |
| Lower bound | 125 | 0 | 63.27 | 100 | 0 |
| Upper bound | 125 | 2 | 63.27 | 100 | 31,635 |
Traveler Contact Data Alternatives
For the less restrictive alternative, HHS/CDC assumes that the process of requesting contact data from airlines and vessel operators would be discontinued. Thus, the cost to provide such data can be modeled as a benefit to airlines and vessel operators equal to their costs under the baseline. For the more restrictive alternative, HHS/CDC assumes that suspension of entry may be implemented for travelers from countries experiencing widespread transmission of quarantinable communicable diseases. Specifically, HHS/CDC assumes that persons traveling from affected countries are not permitted entry to the United States unless such persons spend an amount of time equivalent to the incubation period for the target disease at a location where they are not at risk of exposure and are also screened for symptoms of the disease prior to travel to the United States. During the 2014-2016 Ebola epidemic, travelers from Liberia, Sierra Leone or Guinea would not be able to enter until 21 days in another country or within the affected country but separated from others in a manner that excludes the possibility of interaction with potentially infected individuals.
On average, HHS/CDC has conducted about 2.5 contact investigations for viral hemorrhagic fevers and MERS coronavirus over the past six years. HHS/CDC assumes that if suspensions of entry may be in place, some fraction of these contact investigations may not be conducted.
Thus, the cost to airlines and vessel operators to provide traveler contact data would decrease for the less restrictive alternative resulting in estimated benefits of $94,905. For the more restrictive scenario, the costs are relatively similar as for the NPRM except for subtracting the cost of providing contact data for 2.5 investigations ($15,501 vs. $15,818) and calculating the benefit of doing 2.5 fewer contact investigations each year ($1,898) (Table 10).
| Baseline | NPRM | Less restrictive alternative a | More restrictive alternative b | |
|---|---|---|---|---|
| a The less restrictive alternative is less expensive than the status quo, because HHS/CDC does not request data from airlines and attempt to provide data to health departments to follow up with exposed travelers. | ||||
| b The more restrictive alternative also could potentially reduce costs to airlines and vessel operators because HHS/CDC would restrict travel to countries undergoing widespread transmission of quarantinable communicable diseases such as viral hemorrhagic fevers, MERS or SARS | ||||
| Baseline number of contact investigations | 125 | 125 | 0 | 122.5 |
| Costs | ||||
| Best estimate | NA | $15,818 | $0 | $15,501 |
| Lower bound | NA | 0 | 0 | 0 |
| Upper bound | NA | 31,635 | 0 | 31,002 |
| Benefits | ||||
| Best estimate | NA | 0 | 94,905 | 1,898 |
| Lower bound | NA | 0 | 94,905 | 1,898 |
| Upper bound | NA | 0 | 94,905 | 1,898 |
Change to Definition of an “Ill Person”
HHS/CDC is proposing to update the definition of “ill person” in 42 CFR § 70.1 and 71.1 to better facilitate identification of communicable diseases of public health concern aboard flights and voyages. However, HHS/CDC currently requests that aircrafts and vessels report several of the symptoms included in the revised definition of ill person. Besides aircraft and vessel operators, quarantine stations also receive illness reports from U.S. Customs and Border Protection, U.S. Coast Guard, state and local health departments, and health facilities. These reports are not included in this analysis, which focuses on reporting during travel.
HHS/CDC has crafted the proposed definition of “ill person” in such a way that it should be understood by non-medically trained crewmembers and used to discern illnesses of public health interest that HHS/CDC would like to be made aware of according to 42 CFR 70.4 from those that it does not (e.g., common cold), while more closely aligning the definition with the symptoms reporting guidelines published by ICAO in Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation. To further assist flight crewmembers (and vessel crewmembers under part 71) in identifying individuals with a reportable illness, HHS/CDC provides the following in-depth explanations and examples of the communicable diseases that such signs and symptoms might indicate. Note that these explanations also apply to the definition of “ill person” under part 71.
1. Fever: This term means that the person has a measured temperature of 100.4 °F (38 °C) or greater, feels warm to the touch, or gives a history of feeling feverish. While a measured temperature is the preferable and more accurate method to determine whether a person has a fever, it is not always possible to obtain. The measured temperature also may not reflect the presence of a recent fever, for example, if the individual has taken a fever-reducing medication. For these reasons, the revised “ill person” definition includes other methods that may be used by crewmembers as proxies for a measured temperature. If it is not feasible or advisable to touch the individual or if the individual does not disclose a history of feeling feverish, then, while not definitive, the observer should consider his/her appearance, such as having a flushed face, glassy eyes, or chills as possible indications of the presence of a fever. A self-reported history of feeling feverish is included in the event that the ill person has taken medication that would lower the measured temperature or if the fever fluctuates as part of the natural course of the disease.
2. Skin rash: This term means that the individual has areas on the skin with multiple red bumps; red, flat spots; or blister-like bumps filled with fluid or pus that are intact or partly crusted over. The rash may be discrete or may run together, and may include one area of the body, such as the face, or more than one area. The presence of skin rash, along with fever, may indicate that the traveler has measles, rubella (German measles), varicella (chickenpox), meningococcal disease, or smallpox.
3. Difficulty breathing: This term means that the individual is gasping for air, is unable to “catch” his/her breath, is breathing too fast and shallow to get enough air, or cannot control his/her own secretions. These symptoms may be apparent or self-reported if not obvious. Difficulty breathing, along with fever, may indicate a traveler has tuberculosis, diphtheria, influenza with pandemic potential, or a severe acute respiratory syndrome.
4. Persistent cough: This term means that the cough is frequent and severe enough that it catches the attention of the crewmember, or the individual or another passenger voices concern about it. Persistent cough, along with fever, may indicate the traveler has pertussis/whooping cough (vomiting may occur at the end of a coughing fit), tuberculosis, severe acute respiratory syndrome, or influenza with pandemic potential.
5. Decreased consciousness or confusion of recent onset: This term means that the individual is not fully aware of his/her surroundings or may be unusually difficult to awaken. The individual may appear to be confused or disoriented. Decreased consciousness, along with fever, may indicate the traveler has meningococcal disease, another serious neurological infection, or serious infection in another body system.
6. Bruising or bleeding (without previous injury): This term means that the person has noticeable and unusual bruising or bleeding from gums, ears, nose or areas on skin for which there is no obvious explanation. Unexplained bruising or bleeding, along with fever, may indicate the person has a hemorrhagic fever, such as Ebola, or plague.
7. Persistent diarrhea: This term means that the diarrhea is frequent and severe enough that the air crewmember notices, for example, that the person has been to the restroom numerous times, or the individual or another passenger voices concern about it. Persistent diarrhea may indicate the person has a food or waterborne infection such as norovirus or cholera, or another serious communicable disease, such as Ebola. Many infections that cause persistent diarrhea can be spread easily from person to person, either directly or indirectly through food or water, and cause large outbreaks.
8. Persistent vomiting: This term means that the individual has vomited two or more times (not due to air or sea sickness) and either expresses concern to the air/vessel crew or comes to the attention of others onboard (air/vessel crew or passengers). Persistent vomiting may indicate the person has a food- or waterborne infection such as norovirus, or another serious communicable disease, such as Ebola.
9. Headache with stiff neck: This term means that the individual is self-reporting a headache accompanied by difficulty moving his/her neck. These symptoms may indicate that the individual has bacterial meningitis, such as meningococcal meningitis. Meningococcal meningitis has a high death rate and a significant proportion of survivors have residual impairments, such as deafness or injury to the brain. Individuals in close contact with ill persons with meningococcal disease are at elevated risk for contracting the disease.
The current illness reporting requirements for interstate travel are summarized in 42 CFR § 70.4 and state that “The master of any vessel or person in charge of any conveyance engaged in interstate traffic, on which a case or suspected case of a communicable disease develops shall, as soon as practicable, notify the local health authority at the next port of call, station, or stop, and shall take such measures to prevent the spread of the disease as the local health authority directs.” Communicable disease is defined in 42 CFR § 70.1 as “illnesses due to infectious agents or their toxic products, which may be transmitted from a reservoir to a susceptible host either directly as from an infected person or animal or indirectly through the agency of an intermediate plant or animal host, vector, or the inanimate environment.”
Thus, the changes proposed in this NPRM would amount to fewer illness reports than may be anticipated under the current regulation. However, in practice, according to CDC guidance available at http://www.cdc.gov/quarantine/air/reporting-deaths-illness/guidance-reporting-onboard-deaths-illnesses.html, the symptoms requested for international and interstate illness reporting are the same subset. In addition, according to guidance, reports received by HHS/CDC would be considered sufficient to satisfy the requirement to report to local health departments since HHS/CDC would coordinate any response activities with the local health department after receipt of the illness report.
This NPRM would align the definition from CDC guidance with regulatory text by requiring reports of ill travelers with fever and persistent cough, persistent vomiting, difficulty breathing, headache with stiff neck, decreased consciousness, travelers appearing obviously unwell, or unexplained bleeding. In practice, the codification of such guidance may increase costs to some or all airlines and vessel operators who submit illness reports based only upon symptoms currently identified in 42 CFR 70.1 and not based on CDC guidance. For illness reports from aircraft, FAA may also incur additional costs if the number of illness reports made by aircraft pilots in command to air traffic control and reported to CDC via the Domestic Events Network increases.
For aircraft, the updated definition better aligns with symptoms reporting guidelines published by ICAO in Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation. Therefore, HHS/CDC does not anticipate much additional burden on airlines and vessel operators to report ill travelers during travel.
Although HHS/CDC estimates the net change will be no cost to airline or vessel operators, it may be possible to examine the potential increase using simple assumptions. Table 11 shows the number of reports by pilots in command during flights and recorded in HHS/CDC’s Quarantine Activity Reporting System (QARS). These include reports of illness that fit the illness definition specified in current 42 CFR 71.1, reports based on HHS/CDC’s guidance for airlines and vessel operators, reports made based on the guidelines in Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation, or illness reports unrelated to current regulation or guidance. Such reports can also be subdivided into reports requiring HHS/CDC response (“response reports”) and reports that HHS/CDC receives, but which do not require an HHS/CDC response (“info-only reports”). Info-only reports may include symptoms included in HHS/CDC guidance, but for which the underlying condition can easily be diagnosed not to be a communicable disease of public health concern (e.g., influenza-like illness on an aircraft). Info-only reports can also be based on illnesses not requested by HHS/CDC guidance (e.g., motion sickness). HHS/CDC specifically solicits public comment on cost estimates associated with changes to illness reporting for air and maritime travel and based on the change to the definition of an `ill person’.
| Year/category | Based on symptoms included in current regulation | Based on symptoms included in NPRM | Reports not based on symptoms included in either current regulation or NPRM | Total |
|---|---|---|---|---|
| [HHS/CDC QARS data] | ||||
| In addition to illness reports, HHS/CDC receives an average of 10 death reports during air travel each year. Since death reporting requirements are not changing, these are not analyzed. | ||||
| 2015 | ||||
| Info-only | 30 | 55 | 43 | 128 |
| Response | 33 | 22 | 15 | 70 |
| 2014 | ||||
| Info-only | 33 | 61 | 42 | 136 |
| Response | 19 | 36 | 12 | 67 |
| 2013 | ||||
| Info-only | 31 | 46 | 29 | 106 |
| Response | 21 | 25 | 4 | 50 |
| 2012 | ||||
| Info-only | 34 | 58 | 38 | 130 |
| Response | 12 | 18 | 2 | 32 |
| 2011 | ||||
| Info-only | 27 | 39 | 25 | 91 |
| Response | 25 | 29 | 13 | 67 |
| Average, Info-only | 31 | 51.8 | 35.4 | 118.2 |
| Average Response | 22 | 26 | 9.2 | 57.2 |
| Average, total | 53 | 77.8 | 44.6 | 175.4 |
Table 11 shows that HHS/CDC already receives a number of reports based on symptoms included in HHS/CDC guidance that will be codified with this NPRM. On average, among the total 175 illness reports per year, about 78 annual reports are based on symptoms included in the NPRM, but not in current regulations compared to 53 reports based on symptoms already listed in current regulations. The remaining 45 reports would include those based on fever alone or based on symptoms not included either in current regulatory text or proposed in this NPRM.
The number of illness reports from master of vessels during voyages is summarized in Table 12. Compared to the breakdown in reports for aircraft, the vast majority of illness reports during voyages are for response as opposed to info-only. There may be greater specificity in reports from cruise vessels because of the presence of medical officers onboard vessels. On average, there were about 208 reports requiring follow-up and 10.6 info-only reports each year. In contrast to reports from aircraft, most of the reporting for vessels pertains to symptoms included in the current regulation (175 per year) as opposed to those proposed for this NPRM (32 per year). Very few reports from vessels (3.4 per year) were based on fever only or based on symptoms not included in either current regulation or proposed in this NPRM.
| Year/type of report | Year/category | Based on symptoms included in current regulation | Based on symptoms included in NPRM | Reports not based on symptoms included in either current regulation or NPRM |
|---|---|---|---|---|
| [HHS/CDC QARS Data] | ||||
| In addition to the illness reports reported in the table, HHS/CDC receives about 115 reports of death during maritime travel each year. In addition, HHS/CDC requests, but does not require reporting of influenza-like-illness from cruise vessels (also not included in above table). | ||||
| 2015: | ||||
| Info-only | 5 | 4 | 4 | 13 |
| Response | 179 | 21 | 1 | 201 |
| 2014: | ||||
| Info-only | 6 | 3 | 3 | 12 |
| Response | 168 | 21 | 12 | 201 |
| 2013: | ||||
| Info-only | 1 | 1 | 3 | 5 |
| Response | 145 | 48 | 11 | 204 |
| 2012: | ||||
| Info-only | 5 | 7 | 3 | 15 |
| Response | 167 | 19 | 1 | 187 |
| 2011: | ||||
| Info-only | 1 | 3 | 4 | 8 |
| Response | 196 | 32 | 19 | 247 |
| Average, Info-only | 3.6 | 3.6 | 3.4 | 10.6 |
| Average Response | 171 | 28.2 | 8.8 | 208 |
| Average, total | 174.6 | 31.8 | 12.2 | 218.6 |
When reports are received, public health officers at Quarantine Stations perform case assessments, may request follow-up information, and may consult with CDC medical officers to determine if additional action such as a contact investigation, onboard response, or notification to state and local health departments is warranted. Under one assumed scenario, the change in the definition of “ill person” included in the NPRM could result in a 25% increase in the number of info-only reports. On average, there are 129 info-only reports for aircraft and vessels each year and a 25% increase would correspond to an annual increase of 30 info-only reports on aircraft and 3 info-only reports on vessels (Table 13). If the average time for each report is estimated to be 2 minutes for aircraft pilots in command or masters of vessels to make the report and 60 minutes for HHS/CDC to document the info-only report, the estimated cost of the additional reports can be estimated based on the opportunity cost of time for each type of personnel. In addition to the time required for aircraft pilots in command and masters of vessels to make reports, the FAA may incur additional costs to relay reports to air traffic control through the Domestic Events Network. The amount of FAA staff time is estimated at 26 minutes for a government employee at GS-level 15, step 6 based in Washington DC In reality, there would be three FAA employees involved including 1 GS-15/16 level employee at air traffic control (10 minutes), 1 GS-15 level employee at the Domestic Events Network (10 minutes), and 1 GS-14 level employee at FAA’s Washington Operations Center Complex (6 minutes). [45]
For aircraft pilots in command or masters of vessels (occupation codes 53-2011 and 53-5021), their opportunity cost is estimated from Bureau of Labor Statistics, May 2015 Occupational Employment Statistics [46]based on the average salary of aircraft pilots or copilots ($57.35 per hour) or vessel captain, mate, or pilot ($39.95 per hour). For HHS/CDC employees, the average wage rate is based on the Federal government’s general salary scale for a GS-12, step 5 employee based in Atlanta, GA). Base salaries are multiplied by an overhead multiplier of 100% to account for non-wage benefits and other overhead costs for supporting each employee. The annual quantified costs of 35 additional info-only reports would be $4,586.
| Employee type | Annual change in number of info-only reports | Amount of time required per report (minutes) | Estimated wage rate per hour, USD | Over-head multi-plier (percent) | Estimated cost, USD |
|---|---|---|---|---|---|
| Aircraft: | |||||
| Air or maritime conveyance officer | 30 | 2 | $57.35 | 100 | $115 |
| CDC employee | 30 | 60 | 39.83 | 100 | 2,390 |
| FAA employees | 30 | 26 | 70.57 | 100 | 1,835 |
| Total Cost, aircraft | 4,339 | ||||
| Vessels: | |||||
| Air or maritime conveyance officer | 3 | 2 | 39.95 | 100 | 8 |
| CDC employee | 3 | 60 | 39.83 | 100 | 239 |
| Total costs, vessels | 247 | ||||
| Total costs, aircraft and vessels | 4,586 |
Besides the possible change in costs of info-only reports, the other potential change would be an increase in the number of reports that require HHS/CDC follow-up. Under the most likely scenario, there will not be a change in these reports since the new definition better corresponds to HHS/CDC guidance and to reporting guidelines published by ICAO in Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation. However, there may be an increase in the number of reports requiring a response. Under this scenario, there may be an increase in costs for air or masters of vessels to report illnesses. The increase in reports requiring response is assumed to be 10% of the average annual reports summarized in Tables 10 and 11: 6 reports per year on aircraft and 21 reports per year on vessels. HHS/CDC assumes that the time required to submit illness reports and for FAA staff to relay reports requiring responses is the same as for info-only reports (2 minutes for pilots in command and masters of vessels and 26 minutes for FAA to relay reports, Table 14).
There would likely be no change or a decrease in HHS/CDC costs because earlier reporting would lead to a more efficient HHS/CDC response relative to an alternative in which the illness was later reported by a public health department to HHS/CDC. In addition, the public health response to the illness would likely be more efficient because exposed travelers could be contacted earlier. In rare situations, such travelers may potentially be informed of their potential exposure before disembarking an aircraft or vessel or at the gate after disembarking the aircraft or vessel. Such actions should not result in significant delays by holding travelers on board. In such a situation, monetary benefits could greatly exceed monetary costs ($446) associated with the time required to make and relay the report.
| Employee type | Change in annual number of info-only reports | Amount of time required per report (minutes) | Estimated wage rate per hour | Overhead multiplier (percent) | Estimated cost |
|---|---|---|---|---|---|
| Aircraft: | |||||
| Air or maritime conveyance officer | 6 | 2 | $57.35 | 100 | $23 |
| CDC employee | 6 | 0 | 39.83 | 100 | 0 |
| FAA employees | 6 | 26 | 70.57 | 100 | 367 |
| Total Cost | 390 | ||||
| Vessels: | |||||
| Air or maritime conveyance officer | 21 | 2 | 39.95 | 100 | 56 |
| CDC employee | 21 | 0 | 39.83 | 100 | 0 |
| Total | 56 |
Illness Reporting Alternatives
Illness reporting, contact investigations, quarantine, isolation, and public health measures at ports of entry (e.g., 2014-16 Ebola) are all necessary to improve HHS/CDC’s ability to effectively respond to infectious disease threats. Since this NPRM primarily codifies existing practices, HHS/CDC examines two alternatives: A less restrictive alternative in which HHS/CDC relaxes it regulatory authorities to make compliance voluntary rather than compulsory. Under the more restrictive alternative HHS/CDC may enforce the current requirement that airlines report all persons with communicable diseases to local health departments in addition to reporting to HHS/CDC.
The current status quo for illness reporting is summarized in Tables 11 and 12. Reports can be subdivided by illnesses that fit (1) the ill person definition specified in current 42 CFR 71.1, (2) reports based on HHS/CDC’s guidance for airlines and vessel operators, or (3) illness reports unrelated to current regulation or guidance. As shown in Table 10, only about 53 out of 175.4 (30%) illness reports during air travel appear to be based on symptoms included in the current definition of an ill person in existing 71.1. The remaining 70% of reports are based on symptoms currently requested by HHS/CDC, but not required. In addition, only 67% of illness reports during air travel require HHS/CDC response and follow-up. In comparison, illness reports from vessels are much more likely to be based on the definition of ill person as defined in current 71.1 (174.6/218.6 or 80%). In addition, a much greater proportion of reports require an HHS/CDC follow-up (>95%). This may result from differences in the types of illnesses observed on vessels relative to aircraft or because of the presence of medical officers on cruise vessels, who may be better able to identify communicable diseases of public health concern during travel relative to aircraft personnel.
If illness reporting were entirely voluntary, HHS/CDC assumes the number of reports (both info-only and reports requiring response) would decrease by 50% from both airlines and vessel operators (Tables 11 and 12). HHS/CDC does not have any data to estimate the magnitude of decrease in reporting and requests public comment from airlines and vessel operators to better quantify this reduction. HHS/CDC believes that both HHS/CDC and FAA would continue to maintain their current infrastructure to effectively respond to public health emergencies either on aircraft or vessels. Thus, relative to the status quo, the primary benefits of voluntary reporting would be reduced incremental time costs for pilots in command and masters of vessels, DOT/FAA, and HHS/CDC, especially for info-only illness reports. This 50% reduction in illness reporting would generate cost savings for airlines and vessel operators, HHS/CDC, and DOT/FAA of approximately $11,300 (Tables 15 and 16).
The primary cost for the less restrictive alternative relative to the baseline would be reduced capacity for HHS/CDC to respond quickly to communicable disease threats occurring during travel. This is analyzed in a subsequent section on the health impact of regulated activities.
| Employee type | Change in number of info-only reports | Amount of time required per report | Estimated wage rate | Overhead multiplier (percent) | Estimated cost or benefit |
|---|---|---|---|---|---|
| [Effect on info-only reports] | |||||
| Aircraft: | |||||
| Aircraft Pilots or Copilots | 60 | 2 | $57.35 | 100 | $229 |
| CDC employee | 60 | 60 | 39.83 | 100 | 4,780 |
| FAA employees | 60 | 26 | 70.57 | 100 | 3,670 |
| Air total | 8,679 | ||||
| Vessels: | |||||
| Air or maritime conveyance officer | |||||
| Captains, Mates, and Pilots of Water Vessels | 6 | 2 | 39.95 | 100 | 16 |
| CDC employee | 6 | 60 | 39.83 | 100 | 478 |
| Maritime total | 494 | ||||
| Total (Air + Maritime) | 9,173 | ||||
| Employee type | Change in number of reports requiring response | Amount of time required per report | Estimated wage rate | Overhead multiplier (percent) | Estimated cost or benefit |
|---|---|---|---|---|---|
| [Effect on reports requiring response] | |||||
| Air: | |||||
| Aircraft pilots or copilots | 29 | 2 | $57.35 | 100 | $111 |
| CDC employee | 29 | 0 | 39.83 | 100 | 0 |
| FAA employee | 29 | 26 | 70.57 | 100 | 1,774 |
| Total | 1,885 | ||||
| Maritime illness reports: | |||||
| Captains, mates, and pilots (masters) of vessels | 104 | 2 | 39.95 | 100 | 277 |
| CDC Employee | 104 | 0 | 39.83 | 100 | |
| Total | 277 | ||||
| Tot (Air + Maritime) | 2,162 | ||||
Under the more restrictive alternative, HHS/CDC would require duplicate illness reporting both to HHS/CDC and to local health departments with jurisdiction upon arrival for interstate flights and voyages. This alternative is based upon the existing regulatory text under 42 CFR 70.4. HHS/CDC assumes that 50% of illness reports occur during interstate (relative to international) air travel and that 15% of maritime illness reports occur during interstate travel. The time required for pilots in command and masters of vessels is assumed to be about 4 minutes. This duration is greater than the amount of time estimate for reporting to HHS/CDC because pilots in command and masters of vessels may have to search for contact information for local health departments and because local health departments may have less experience dealing with illness reports than HHS/CDC. The costs to airlines and vessel operators is estimated to be $848 per year (Table 17). Since HHS/CDC would coordinate responses to illness reports with local health departments under the status quo, there are no additional costs or benefits to requiring duplicative reports to local health departments. These costs would be added to the costs of the changes resulting from the NPRM.
| Employee type | Change in number of info-only reports | Amount of time required per report | Estimated wage rate | Overhead multiplier | Estimated cost or benefit |
|---|---|---|---|---|---|
| Aircraft pilots or copilots | 88 | 4 | $57.35 | 100% | $673 |
| Captains, mates, and pilots (masters) of vessels | 33 | 4 | 39.83 | 100% | 175 |
| Total | 848 |
The monetized annual costs resulting from the change in the definition of “ill person” are summarized in Table 18.
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| a For the less restrictive scenario, the current reporting requirement is relaxed leading to a reduction in costs. | |||
| Costs | |||
| NPRM: | |||
| Aircraft | $ 4,729 | ||
| Vessels | 303 | ||
| Total | 5,032 | ||
| Less Restrictive Alternative: a | |||
| Aircraft | |||
| Vessels | |||
| Total | |||
| More Restrictive Alternative: | |||
| Aircraft | $ 673 | $ 673 | 5,402 |
| Vessels | 175 | 175 | 478 |
| Total | 848 | 848 | 5,880 |
| Benefits | |||
| NPRM: | |||
| Aircraft | |||
| Vessels | |||
| Total | |||
| Less Restrictive Alternative: a | |||
| Aircraft | 10,563 | 10,563 | 10,563 |
| Vessels | 771 | 771 | 771 |
| Total | 11,334 | 11,334 | 11,334 |
| More Restrictive Alternative: | |||
| Aircraft | |||
| Vessels | |||
| Total | |||
The total costs of the proposed NPRM are summarized in Table 19 and include the costs of the change to the definition of an “ill person” and the codification of the requirement for airlines to provide passenger contact data for the NPRM, the less restrictive alternative, and the more restrictive alternative.
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| Costs | |||
| NPRM: | |||
| 71.4 and 71.5 Passenger data collection | $15,818 | $0 | $31,635 |
| 70.1 and 71.1 Change in definition of an “ill person“ | 0 | 0 | 5,032 |
| Total costs | 15,818 | 0 | 36, 667 |
| Less Restrictive Alternative: | |||
| 71.4 and 71.5 Passenger data collection | 0 | 0 | 0 |
| 70.1 and 71.1 Change in definition of an “ill person“ | 0 | 0 | 0 |
| Total costs | 0 | 0 | 0 |
| More Restrictive Alternative: | |||
| 71.4 and 71.5 Passenger data collection | 15,501 | 0 | 31,002 |
| 70.1 and 71.1 Change in definition of an “ill person“ | 848 | 848 | 5,880 |
| Total costs | 16,349 | 848 | 36,883 |
| Benefits | |||
| NPRM: | |||
| 71.4 and 71.5 Passenger data collection | 0 | 0 | 0 |
| 70.1 and 71.1 Change in definition of an “ill person“ | 0 | 0 | 0 |
| Total benefits | 0 | 0 | 0 |
| Less Restrictive Alternative: | |||
| 71.4 and 71.5 Passenger data collection | 94,905 | 94,905 | 94,905 |
| 70.1 and 71.1 Change in definition of an “ill person“ | 11,334 | 11,334 | 11,334 |
| Total benefits | 106,239 | 106,239 | 106,239 |
| More Restrictive Alternative: | |||
| 71.4 and 71.5 Passenger data collection | 1,898 | 1,898 | 1,898 |
| 70.1 and 71.1 Change in definition of an “ill person“ | |||
| Total benefits | 1,898 | 1,898 | 1,898 |
Benefits from streamlining the CI process for routinely imported diseases
This section reports the benefits that HHS/CDC anticipates from implementation of the NPRM in avoiding the costs incurred annually for CIs of infectious diseases. The primary steps of CIs for routine diseases are:
- A traveler (the index case) is identified as ill either during the flight or voyage with a reportable illness or after with a notifiable disease. The aircraft pilot in command or master of vessel may report the illness directly to HHS/CDC. Illnesses on aircraft may also be reported indirectly to HHS/CDC via air traffic control and then through the Domestic Event Network. If the report occurs after travel, a healthcare facility would then report the illness either to HHS/CDC or public health departments (Ph.D.s).
- If CI criteria are met, HHS/CDC contacts the airlines for
○ a manifest to determine where the index case was seated in relation to other passengers or crew members,
HHS/CDC also asks the airlines for traveler contact information
HHS/CDC then requests information available in multiple DHS’ databases to verify or obtain passenger contact information not included in the manifest.
Once HHS/CDC has the traveler contact information and flight-seating chart, the CI begins. Current CI procedures are cumbersome, primarily because of the difficulties associated with obtaining traveler contact information. HHS/CDC staff may contact airlines more than once to obtain traveler contact data including email address, one or two phone numbers, and address in the United States for U.S. citizens and permanent residents. Because of missing or incorrect contact data from airlines, HHS/CDC also works with DHS to access contact information for travelers exposed to communicable diseases on international flights.
When passenger contact information is delayed or partial, state/local public health departments are delayed in starting CIs and, depending on the disease, this delay could make it impossible to prevent illness and/or the transmission of disease. Further, PHDs have less success contacting passengers with partial information than they would if airlines’ and vessel operators’ compliance with requests was improved as a result of this NPRM.
The model for estimating the benefits of CIs is: Current number of CIs × (reduction in HHS/CDC and health department staff time/resources per contact) × value of staff time.
The rest of this section reports both the quantifiable benefits arising from streamlining the CI process and a discussion of health benefits that can be substantial but cannot be directly quantified on an annual basis. The differential impacts of the various diseases make it hard to summarize NPRM effects given uncertainty around future probabilities of case(s) of multiple such notifiable disease(s). Instead, HHS/CDC presents a simple example based on the average PHD costs associated with a measles outbreak in case such an outbreak could be avoided as a result of either improved illness reporting onboard conveyances or as a result of improved compliance with HHS/CDC requests for traveler contact data.
Estimating the number of infected travelers.
Most air travelers with illness are not identified in flight, but rather seek medical care and are identified as an index case after their travel is completed. Since travelers spend more time on vessels during maritime trips, more illnesses are detected during voyages and contact investigations may be implemented on board vessels. When illnesses are detected after travel, the medical practitioner should notify HHS/CDC or a PHD if the diagnosed disease is on either the list of quarantinable communicable diseases or the list of notifiable diseases. If HHS/CDC can draw upon the improved contact information based on the codification of requests for traveler contact data to aircraft and vessel operators as set forth in this NPRM to locate travelers exposed to an index case before he/she becomes ill, the risk of onward disease transmission can be reduced. By contacting ill travelers more quickly, HHS/CDC may slow the spread and the severity of the outbreak. The benefits therefore depend on:
- How many infected travelers are expected to enter the United States;
- How many quarantinable or notifiable diseases are detected either on-board the aircraft/vessel or reported to HHS/CDC by PHDs;
- How many exposed travelers will become ill as a result of exposure during travel;
- How the infection will be transmitted within the U.S. population;
- How effective public health agency contact tracing will be with and without the NPRM.
In addition to improved efficiencies associated with more timely or more complete provision of traveler contact data by airlines and vessel operators, there may also be an increase in the number of reports of ill travelers during travel that require HHS/CDC follow-up. Under the most likely scenario, there will not be a change in these reports, since the new definition better corresponds to reporting guidelines published by ICAO in Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation and current HHS/CDC guidance. However, as reported in Table 13, there may be an increase of 23 reports requiring a response during flights and voyages. Under this scenario, there would likely be no change or a decrease in HHS/CDC costs because earlier reporting would lead to a more efficient public health response relative to an alternative in which the illness was later identified after presentation to a health care provider and reported by a Ph.D. In addition, the public health response to the illness would likely be more efficient because exposed travelers could be contacted earlier, potentially before disembarking the aircraft or vessel.
Primary benefits: Improved efficiency of contact investigations undertaken by CDC and partners at state and local health departments and reduced risk of infectious disease outbreaks
The primary monetized annual benefit for both the change to the definition of an “ill person” for the purposes of illness reporting and the codification of HHS/CDC requests from airlines and vessel operators for traveler contact data is an improvement in CDC’s ability to respond effectively and mitigate infectious disease outbreaks. There are a number of intermediate steps between either an illness report or receiving more complete or timelier traveler data and stopping an infectious disease outbreak. For example, the travelers exposed to the infectious disease would have to comply with public health measures to mitigate either their risk of becoming ill with a specific infectious disease or transmitting that disease to other individuals.
The amount of time HHS/CDC staff spent per air or maritime contact varies with the size of the CI because some tasks are CI-specific, such as filling out reports or obtaining manifests, and some are contact-specific such as determining a specific traveler’s contact information. The CI-specific labor time costs less per contact when an investigation includes more contacts, e.g., a manifest that takes 60 minutes of CDC staff time to obtain for 2 contacts is the equivalent of 30 minutes-staff-time-per-contact while the same manifest listing 30 contacts is the equivalent of 2 minutes-staff-time-per-contact. On the other hand, the traveler-specific time tends to increase-per-contact with less information and decrease-per-contact with more information. [47]Further, the QARS system used to document and follow up on CIs requires full-time personnel to maintain the system, pull regular reports, and monitor follow-up of travelers contacted during CIs. Finally, HHS/CDC has two full-time persons regularly assigned as liaisons to DHS whose duties include gathering contact information from DHS systems. Therefore, for HHS/CDC staff time to initiate and follow up on different sized CIs, to track down traveler contact information from multiple sources, to work with PHDs, document and report on CIs, update and train in systems, and manage the staff involved in CIs, a cost of $180 per contact is estimated. This is the equivalent of 2 hours of a HHS/CDC staff person’s being paid the salary of a GS-13, step 4 plus 100% for benefits and employee overhead costs (Table 20).
For PHD resources, HHS/CDC also estimated a cost-per-contact of $180, which is consistent with HHS/CDC costs and a recent publication adjusted to 2015 dollars. [48] PHD processes vary greatly from state to state and at the local level within a state. A couple of examples:
- One state assigns 2 registered nurses (RNs) who perform 5 CIs or fewer per year for the entire state another state assigns 3 RNs, a Public Health Service Medical Officer, a physician, and a data analyst and conducts about 25 CIs a year [49]
- When one state receives information about passenger contacts from HHS/CDC, the state epidemiologist creates several documents to fax to the relevant county health departments, a team of an epidemiologist and RNs at the county then either call or visit the contacts if there is an address. But the state epidemiologist will make every effort to locate travelers even if their final destination is unclear. [50]
Finally, different diseases may elicit different levels of response at the PHD level, with a more rapid response for highly infectious diseases like measles that can be prevented with timely post-exposure prophylaxis and a more measured response for less infectious diseases like TB. By using the same cost for HHS/CDC and for PHDs, HHS/CDC believes the potential cost savings from reduced effort for PHDs to locate infectious disease contacts are conservatively estimated.
| CDC | PHD |
|---|---|
| $180 | $180 |
HHS/CDC obtained the total number of contacts traced (2,715 per year, Table 6) for all diseases reported on international flights. International flight data were extracted for this analysis because the codification of the requirements to provide timelier and more complete contact data is expected to have the greatest impact on HHS/CDC and PHD activities and potential benefits. In comparison, HHS/CDC requests contact information for approximately 664 contacts per year on interstate flights (Table 7). HHS/CDC also supports contact investigations affecting an average of 762 contacts per year for illnesses on board vessels (Table 8); however, many of these investigations occur before travelers disembark vessels. By limiting the analysis to contacts on international flights, HHS/CDC conservatively estimates the potential benefits associated with this NPRM. HHS/CDC multiplied the average annual number of contacts on international flights by the cost-per-contact for HHS/CDC and PHDs (Table 20) to estimate the costs of CIs under the current baseline.
To estimate the benefits (Table 21), HHS/CDC assumed a percent reduction in staff time for CIs at HHS/CDC (0-5%) and PHD levels (0-3%) based on internal conversations with personnel directly involved in the CI process. The reduction in staff time that would result from implementation of this NPRM would arise from the ability of HHS/CDC to have a better starting point with which to provide traveler contact data to state and local health departments as a result of the receipt of more complete and timely traveler contact data from airlines. This would improve HHS/CDC’s ability to transmit information to destination states more quickly and for states to contact exposed travelers earlier. This would allow states to start their investigations more quickly, contact more travelers faster to conduct public health assessments and potentially offer preventive medications or vaccines in a more timely fashion. In addition, it would be less likely that HHS/CDC would send incorrect contact data to states. With all of the preceding factors in mind, HHS/CDC estimated that the NPRM would reduce labor time by between 0% to 5% at CDC, and 0% to 3% at PHDs. The higher percentage of avoided costs at HHS/CDC reflect reduced efforts by HHS/CDC to search for accurate contact data for travelers due to untimely or inaccurate data provided by airlines. The lower percentage of avoided costs at PHDs reflects a more diffuse (e.g.,multiple local PHDs in a state) infrastructure and the more labor-intensive tasks of following up on individuals. These estimates should be conservative if there is a substantial improvement by airlines in responding to requests for traveler contact data or if the change to the definition of “ill person” leads to more reports of ill travelers during travel.
HHS/CDC annual costs to engage in international air, interstate air, and maritime CIs are about $745,000 or roughly the equivalent of 3.8 HHS/CDC full-time employees (FTEs) at the wage level of GS-13, step 4 plus benefits and overhead (Table 21). The NPRM should have the greatest effect on the international air CIs. The annual reduction in contact tracing costs from implementing the NPRM (Table 22) for HHS/CDC ranged from $0 to $24,435 based on a 0-5% reduction in effort on international CIs. For PHDs, the reduction in costs ranged from $0 at the lower bound to $14,661 at the upper bound (Table 22).
| Annual # contacts | CDC | PHD costs | Total costs | |
|---|---|---|---|---|
| CDC and PHD Baseline Costs (Current Practice) | ||||
| International air contacts | 2,715 | $488,700 | $488,700 | $977,400 |
| Interstate air contacts | 664 | 119,520 | 119,520 | 239,040 |
| Maritime contacts | 762 | 137,160 | 137,160 | 274,320 |
| Total baseline costs | 4,141 | 745,380 | 745,380 | 1,490,760 |
| Viral hemorrhagic fever, MERS, and SARS contacts | 163 | 29,340 | 29,340 | 58,680 |
| CDC and PHD Baseline Costs (Current Practice) | ||||
| Annual # contacts | CDC | PHD | ||
| International contacts | 2,715 | $488,700 | $488,700 | |
| CDC and PHD Costs with the NPRM | ||||
| Estimated costs for HHS/CDC after efficiency improvement with NPRM | Estimated costs for PHDs after efficiency improvement with NPRM | |||
| 0%, Lower bound | 5%, Upper bound | 0%, Lower bound | 3%, Upper bound | |
| International contacts costs assuming reduction in time (2,715) | $488,700 | $464,265 | $488,700 | $474,039 |
| Benefits from Implementing the NPRM | ||||
| CDC 0% and 5% reduction in effort | PHD 0% and 3% reduction in effort | |||
| Benefits (Reduced costs) | $0 | $24,435 | $0 | $14,661 |
The best estimate of benefits are the midpoint of the lower bound and upper bound estimates for both HHS/CDC and PHDs ($19,548). The lower bound ($0) and upper bound estimates ($39,096) for both entities are also reported in Table 23.
| HHS/CDC benefits | PHD benefits | Total | |
|---|---|---|---|
| Best estimate | $12,218 | $7,331 | $19,548 |
| Lower bound | 0 | 0 | 0 |
| Upper bound | 24,435 | 14,661 | 39,096 |
The total annual monetized benefits by stakeholder from the potential reduced effort for contact investigations are summarized in Table 24.
| HHS/CDC benefits, USD | PHD benefits, USD | Airlines, USD | Total | |
|---|---|---|---|---|
| Best estimate | $12,218 | $7,331 | $0 | $19,548 |
| Lower bound | 0 | 0 | 0 | 0 |
| Upper bound | 24,435 | 14,661 | 0 | 39,096 |
For the less restrictive alternative, the change relative to baseline is equal to the current cost of performing CIs ($745,000 each for HHS/CDC and local health departments or a total of about $1.5 million). Under the more restrictive alternative (i.e. implementing travel restrictions immediately upon evidence of widespread transmission of viral hemorrhagic fevers, SARS or MERS, the costs of these contact investigations are assumed to be avoided (potential savings to HHS/CDC of about $29,000 each or $59,000 in total). The benefits of the avoided contacted investigations are then added to the cost savings for the remaining contacts assuming a 0-5% improvement in HHS/CDC efficiency and a 0-3% improvement in Ph.D. efficiency as for the NPRM (Table 25).Show citation box
| HHS/CDC benefits | PHD benefits | Total | |
|---|---|---|---|
| NPRM | |||
| Best estimate | $12,218 | $7,331 | $19,548 |
| Lower bound | 0 | 0 | 0 |
| Upper bound | 24,435 | 14,661 | 39,096 |
| Less Restrictive Alternative: | |||
| Best estimate | 745,380 | 745,380 | 1,490,760 |
| Lower bound | 745,380 | 745,380 | 1,490,760 |
| Upper bound | 745,380 | 745,380 | 1,490,760 |
| More Restrictive Alternative: | |||
| Best estimate | 41,558 | 36,671 | 78,228 |
| Lower bound | 29,340 | 29,340 | 58,680 |
| Upper bound | 53,775 | 44,001 | 97,776 |
Potential Reduction in Costs of Infectious Disease Outbreaks
For some diseases, there is empirical data from which on board transmission can be estimated. According to a published analysis of the outcomes of measles contact investigations (74 case-travelers on 108 flights resulting in 3,399 contacts) in the United States between December 2008 and December 2011, HHS/CDC could not assign 9% of measles contacts (322) to a health department due to insufficient contact data. Another 12% of these contacts (397) were believed to be outside the United States. [51] After HHS/CDC provides contact data to state health departments, HHS/CDC requests, but does not require health departments to provide data on the outcomes of their attempts to follow-up with travelers. Among the 2,673 contacts assigned to U.S. public health departments in 2008-11, HHS/CDC only received outcome data for 1,177 out of the 2,673 assigned contacts. This outcome data included reports from state health departments that 225 out of the 1,177 assigned contacts could not be located (19%). Among the 952 contacts for which HHS/CDC received measles outcome data from health departments, there were 9 lab-confirmed measles cases (1%). Since there may be reporting bias from health departments (i.e. health departments would be more likely to report outcome data for contacts that developed measles than for other exposed travelers that did not develop measles, HHS/CDC considers a range of measles incidence rates among exposed travelers from 9 cases/2,673 contacts assigned to health departments (0.34%) to 9 cases/952 exposed contacts with outcome data reported to HHS/CDC (0.95%). This probability could overstate or understate the true transmission rate depending on the length of the flight and seating configuration. On the other hand, it may understate the probability if cases were not reported or occurred overseas.
The majority of travelers exposed to measles on aircraft (~74%) had pre-existing immunity based on past measles immunization, past measles illness, or being born prior to 1957 and thus likely to have measles immunity even if they do not recall experiencing the disease.[52] Among the 952 exposed travelers, 8 cases occurred in the 247 contacts (3.2%) without known pre-existing immunity compared to 1 case in the 705 contacts with past history of vaccination or measles illness (0.1%). The median age of measles cases was 1.6 years.
Intervention by public health departments mitigates the risk of measles transmission in two ways. First, exposed travelers without measles immunity may be offered post-exposure prophylaxis with measles-containing vaccine (within 72 hours) or immune globulin (within 6 days), [53] which can prevent onset of disease, halting outbreaks before they begin. Under the status quo, relatively few exposed travelers receive post-exposure prophylaxis (just 11 out of 248 travelers with no history of measles immunization or infection). Second, exposed travelers would be counseled by health departments to self-isolate and seek treatment if they started to experience symptoms consistent with measles onset. For example infants exposed during travel and too young to be vaccinated could arrange for special precautions if they visit a pediatrician after becoming ill with measles-like symptoms to minimize the transmission to other unvaccinated infants. Both activities will limit the possibility of measles transmission to family members or others in the community. The attack rate for measles is estimated to be 90%, but the high background immunization rate and high efficacy of measles vaccine attenuates the burden of measles outbreaks in the United States.
In summary, the potential size of a measles outbreak occurring depends on:
- The number of persons contacted by the infectious measles patient
- Background immunity among persons contacted
○ Survey estimates have shown considerable heterogeneity in background vaccination rates such 80% of unvaccinated children live in counties comprising 40% of the total population. [54]
For tuberculosis, it is difficult to estimate the transmission rate on an aircraft or vessel. A modeling study suggests that the risk of infection is about 1/1000 on an 8.7 hour flight and that persons seated closer to the index case are at greater risk of infection. [55] Only 5-10% of persons infected with the bacteria Mycobacterium tuberculosis will go on to develop active, infectious disease and the risk of progression is greatest within the first two years after infection. [56]
An analysis of the epidemiology and outcomes of CDC-led flight-related tuberculosis contact investigations conducted in the United States from January 2007 to June 2008 involved 131 case-travelers and 4,550 passenger-contacts. [57] Among 3,375 (74%) passenger-contacts whose information was provided to health departments, HHS/CDC received results for 861 (26%). HHS/CDC found that 103/861 (12%) had a previous history of a positive TB screening test result or treatment for latent tuberculosis or active disease and were not re-tested. Of the remaining 758 passenger contacts, 182 (24%) tested positive. The majority of travelers with data about TB risk factors (other than exposure to cases during air travel) had at least one risk factor (130/142 or 92%). Risk factors included having been born or lived in a country with high TB prevalence (prevalence > 100 per 100,000 population). Although passenger-contacts with risk factors were more likely to have pre-existing latent tuberculosis infection, the authors could not exclude the possibility that infection was acquired during the flights when the travelers were exposed. Furthermore, because outcomes data were reported for only 26% of passenger contacts forwarded to US health departments (19% of all passenger contacts) the precise determination of in-flight transmission risk of M. tuberculosis was not feasible. [58]
The results from this investigation were used in a cost-effectiveness study to estimate the return on investment for tuberculosis CIs. The authors examined a range of latent tuberculosis prevalence rates among exposed travelers that varied between 19% to 24% for two different HHS/CDC CI protocols for flight-related TB investigations. The return on investment was calculated based on the likelihood that travelers with latent tuberculosis infection would initiate and complete a treatment regimen to clear the infection, the average cost of tuberculosis treatment, a tuberculosis case fatality rate of 5% and a conservative value of statistical life estimate of $4.2 million (in 2009 USD) to account for the value of mortality risk reduction from avoided tuberculosis disease. The return on investment depended on the probability assumed for persons with latent TB infection to develop active disease (5-10%) and variation in the costs to health departments to locate exposed travelers ($28 to $164). Using the expected latent tuberculosis prevalence rate of 19% in travelers identified for contact investigations on flights and a health department cost per contact of $164, the return on investment was estimated to vary between $1.01 and $3.20. The return on investment formula was calculated based on (Expected benefits − Expected costs)/Expected costs. Thus, for each $1 spent on contact investigations (including Federal and state resources) and offering treatment to persons infected with latent tuberculosis infections would result in benefits in excess of costs equal to $1.01 to $3.20 59 60 on average. At the upper bound latent tuberculosis prevalence estimate (24%), the return on investment was estimated to vary between $1.35 and $3.92.
There is also empirical data for SARS infections occurring on an aircraft. A study reported that 37 infections resulted from 40 flights with infectious passengers on board. Of the 40 flights, four have documented aircraft sizes. They average 127 passengers per plane. [61]Therefore the on board transmission rate could be estimated to be 0.73% among all travelers. In comparison, there is no evidence of transmission of MERS Coronavirus or viral hemorrhagic fevers during travel on aircraft or vessels. However, there have not been enough observations to determine that there is no risk.
For the remainder of the diseases, empirical data does not exist. Like measles, immunizations are recommended to prevent pertussis, rubella, and meningococcal disease. Since meningococcal conjugate vaccine was more recently added to the United States vaccination schedule, it is likely that background immunity is much lower relative to measles, rubella or pertussis.
In the absence of data for some diseases, the infection rate of measles is used to estimate the infection rates by using the ratio of basic reproduction numbers (R 0). The basic reproduction number is a measure of disease infectiousness. Specifically, it is an estimate of new infections in a completely susceptible population. For example, rubella has an R 0 of 9 to 10 while measles has an R 0 of 15 to 17. [62] The infection rate of measles is multiplied (0.0034 to 0.0095) by the ratio of the average basic reproductive numbers (9.5/16) to arrive at a transmission rate (0.002 to 0.006) for rubella on airplanes. This rate is approximately 60% of the rate for measles. The estimated transmission rates for some diseases are reported in Table 26. The exceptions are for meningococcal disease and tuberculosis. For meningococcal disease, the risk of transmission in household contacts 0.002 to 0.004 [63] is used in the absence of other data and taking account that CIs are only performed for travelers sitting adjacent to the index case or in the event of other known exposures. For tuberculosis, the probability that exposed travelers have latent tuberculosis [64] (19%-24%) is used, although infection may have occurred prior to air travel. For the purposes of evaluating the economic impact of tuberculosis investigations, it does not matter if travelers were infected during travel or before.
| Disease | R 0 | Estimated transmission rate on aircraft to exposed passengers | |
|---|---|---|---|
| Lower bound | Upper bound | ||
| Diphtheria | 11 to 14 | 0.0026 | 0.0074 |
| Measles | 15 to 17 | 0.0034 | 0.0095 |
| Meningococcal Disease | NA | <2/1000 | <4/1000 |
| Pertussis | 4 to 5 | 0.001 | 0.003 |
| Rubella | 9 to 10 | 0.002 | 0.006 |
| TB | NA | 0.19 | 0.24 |
Estimated Number of Cases in Traveler Contacts
The number of potential contacts for each disease can be multiplied by the estimated transmission rate by disease in Table 26 to generate a rough estimate of the annual number of cases among traveler contacts. These numbers of contacts for each disease are summarized in Tables 6 and 7 for interstate and international CIs respectively. Contact investigations on vessels are excluded for this analysis. Based on this analysis, tuberculosis (19 to 48) and measles cases (3.6 to 10.1) are the most likely diseases that will be diagnosed among contacts exposed during travel (Table 27). Tuberculosis contact investigations only occur for international flights with the very rare exception of a domestic flight with a duration greater than 8 hours. The numbers of contacts and outcomes are much more uncertain for other diseases. The number of tuberculosis cases are adjusted from the number of contacts with tuberculosis by assuming that only 5% (lower bound) to 10% (upper bound) of infected contacts will go on to develop clinical disease. [65]
For viral hemorrhagic fevers and MERS, there is no evidence of transmission, but there have not been very many observations. The costs of a MERS outbreak in South Korea and U.S. Ebola cases are presented in another section of the RIA that analyzes the economic impact of the Ebola Enhanced entry risk assessment and management program.
| Passengers per flight | Number of contacts | Expected incidence among contacts (lower bound) | Expected incidence among contacts (upper bound) | Expected number of new cases (lower bound) | Expected number of new cases (upper bound) |
|---|---|---|---|---|---|
| a For tuberculosis, travelers contacts are typically found to test positive for infection, but do not have active disease. | |||||
| b These probabilities indicate the likelihood that a contact will test positive for infection. | |||||
| c The expected numbers of case adjust for the finding that only 5-10% of individuals that test positive for infection will go on to develop clinical disease. | |||||
| MERS Coronavirus | 101 | Insufficient data | |||
| Measles | 1069 | 0.0034 | 0.0095 | 3.6 | 10.1 |
| Meningococcal Disease | 1.7 | 0.00200 | 0.00400 | 0.0033 | 0.0067 |
| Pertussis | 16.8 | 0.001 | 0.003 | 0.02 | 0.04 |
| Rubella | 117 | 0.002 | 0.006 | 0.2 | 0.7 |
| TBa | 1,995 | b 0.19 | b 0.24 | c 18.9 | c 47.90 |
| Viral Hemorrhagic Fever | 62.0 | Insufficient data | |||
| Total | 3,362 | 22.8 | 58.7 | ||
These estimates of cases may be a lower bound, because potential cases resulting from flights in which contact investigations were not performed are not included. Especially for tuberculosis cases, many international travelers may return to their home countries before seeking treatment and such cases may not lead to contact investigations if HHS/CDC is not informed.
Impact of NPRM—Measles
On average, HHS/CDC identified 564 travelers exposed to measles cases on international flights during 2010-2015 (Table 6). The NPRM may affect the cost for health departments to implement public health measures in two ways: (1) Health departments may contact exposed travelers more quickly and (2) health departments may be able to contact a higher percentage of exposed travelers. For the first set of travelers that are contacted earlier with the NPRM than under the status quo, the cost to both the contacted travelers and to health departments should be less than under the status quo. For measles contacts, earlier follow-up with public health departments should lead to more travelers receiving measles vaccines within 72 hours. This would potentially reduce the cost of following up with exposed travelers or to administer immune globulin or to monitor travelers that have been located after the 72-hour window in which measles vaccination would reduce their risk of developing symptomatic measles. At present, very few travelers receive post-exposure prophylaxis, 11/248 or 4.4%. [66] In addition, health departments have implemented quarantine (usually voluntary) for unvaccinated, high risk measles exposures. [67] HHS/CDC notes that measles vaccine is recommended for all persons lacking immunity. Thus, the costs of vaccination for exposed travelers as part of the contact investigation may have been incurred at a later date if travelers’ health care providers recommended measles vaccination at a more routine health care visit in the future. [68] However, to be conservative, HHS/CDC includes the full additional cost to administer such vaccines to persons contacted.
Among the contacts, HHS/CDC estimates that approximately 25% (141 contacts per year) cannot be located by public health departments (Table 28), either because HHS/CDC cannot assign the contacts to health departments or because the information provided by HHS/CDC is not sufficient to enable health departments to locate contacts after assignment from HHS/CDC. Among these contacts, HHS/CDC assumes that 10% of all contacts (56) are not located because HHS/CDC cannot assign contacts to state health departments due to insufficient data. For these contacts, health departments would not incur any contact tracing costs because such contacts would not be assigned. HHS/CDC assumes a 15% improvement from baseline as a result of this NPRM (Table 28). This would result in 8.5 additional contacts per year assigned to health departments for contact tracing. As shown in Table 20, HHS/CDC estimates that health departments incur an estimated cost of $180 per contact. The marginal cost incurred from this NPRM for additional measles contacts assigned to health departments would be $180 × 8.5 = $1,530 per year (Table 29).
| Description | n | Reference |
|---|---|---|
| Average contacts per year for measles, (a) | 564 | Table 6. |
| Estimated number of contacts for which HHS/CDC cannot assign to a health department, (b) = 10% × (a) | 56 | Nelson et al. 2013 69. |
| Estimated improvement in HHS/CDC’s ability to assign contacts to health department (c) = 15% × (b) | 8.5 | Assumption. |
| Numbers of people who are not currently contacted due to lack of contact information, (d)=(a) × 25% | 141 | Nelson et al. 2013. |
| Expected numbers of people who could be contacted with NPRM, (e) = (d) × 15% | 21 | Assumption. |
| Among those contacted, 70% would have evidence of measles immunity (f) = (e) × 70% | 15 | Nelson et al. 2013 (Table 2). |
| Among those contacted, 30% may be susceptible to measles (g) = (e) × 30% | 6 | Nelson et al. 2013 (Table 2). |
| Number of additional names sent to health department, (c) | 8.5 |
| Additional cost per contact to health department to search for and examine contacts (USD per contact) (h) | $180 |
| Additional cost to health department to search for contacts, total (USD), (i) = (c) x (h) | $1,530 |
| MMR vaccine price per dose (USD) (j) | $39 |
| Vaccine administration cost (k) | $31 |
| Estimated cost prophylactic measles vaccine per person (USD), (l) = (j) + (k) | $70 |
| Number of individuals requiring measles vaccine, (g) | 6 |
| Cost of measles vaccination, total (USD) (m) = (g) x (l) | $420 |
| Total additional annual cost to follow up with more contacts (USD), (i) + (m) | $1,950 |
In addition, HHS/CDC assumes that the NPRM could improve health departments’ abilities to contact 15% of those who could not be currently contacted because of insufficient contact information (21 contacts per year). Among the 21 additional exposed travelers that would be contacted, 70% of them (15 per year) are expected to have measles immunity because they were born before 1957, had history of measles, or received one or more doses of measles vaccine. The remaining 6 travelers per year without proven measles immunity would incur additional costs to be vaccinated (Table 29).
To be conservative, HHS/CDC assumes that all 6 exposed travelers would be adults and would be vaccinated with the measles-mumps-rubella (MMR) vaccine. The vaccine price for adults is estimated from the Vaccines for Children vaccine price archives (July 2014 and July 2015) [70] based on the public sector price for the vaccine. Vaccine administration costs are estimated from Healthcare Solutions’ 2015 Physicians’ Fee & Coding Guide (CPT 90471). [71] Total costs to vaccinate 6 people are estimated to be $420 at $70 per person vaccinated. Total costs resulting from the NPRM are summarized in Table 30.
| Net cost for measles investigations | Additional names provided to health departments | Addition contacts reached by health departments | Number of travelers provided post-exposure prophylaxis | Number of travelers identified earlier | Average probability that contact is infected |
|---|---|---|---|---|---|
| $1,950 | 8.5 | 21 | 6 | Unknown | 0.0035—0.0095 |
Baseline Measles Burden
In the absence of interventions by public health departments, travelers infected with measles during international travel would be as likely as any other individuals to spark a measles outbreak. In fact, travelers exposed during international travel may be more likely to visit a high traffic tourist destination leading to more exposures than the average measles case in the United States. In the absence of HHS/CDC efforts to retrieve and transmit contact data, public health departments would not be able contact travelers to provide post-exposure prophylaxis and to self-monitor for potential measles symptoms.
For measles in 2011, 16 outbreaks occurred leading to 107 cases. An outbreak was defined based on 3 or more cases in a cluster. [72] The remaining 113 cases reported in 2011 resulted in one or two cases per cluster. Thus, the probability that any individual measles index case leads to an outbreak was between 16(16+113) = 12.4% and 16/(16+57) = 20.1%. The lower bound represents an assumption that all of the 113 cases unassociated with outbreaks of 3 or more cases occurred in clusters with just one case each. The upper bound represents a scenario with 56 clusters of two cases each with one cluster with one case. Thus, the probability that any individual measles case could spark an outbreak of 3 or more cases is 12.4% to 20.1%. The average cost to public health departments per measles outbreak is $250,000 and the upper bound cost is $1 million. [73]
HHS/CDC assumes that the probability that measles case resulting from exposure during travel and that is not contacted by a public health department is as likely as any other measles case to initiate a measles outbreak of 3 or more cases, which occurs at an approximate probability of 12.4% to 21.9%. The average cost to health departments is $250,000 for each of these outbreaks and the average outbreak size is about 7 cases (107 cases/16 outbreaks).
The estimated illness costs for measles are $300 ($86-$515) for outpatient cases and $24,500 ($3,900-$45,052) for inpatient cases. [74]The probability of hospitalization is estimated to be 44.3%. [75] A range of hospitalization rates is estimated based on 50% to 150% of this base case estimate (22%-66%). The measles case fatality rate has been estimated to be 0.2%. [76] HHS/CDC assumes that the value of statistical life is $9.4 million (range $4.3 million to $14.2 million). This value is an estimate of the average willingness to pay to reduce one’s mortality risk by a small increment not an estimate of the value of any specific person’s life. Using these estimate the average illness costs associated with a measles case (Table 31) is about $30,000 ($9,500 to $58,000).
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| Outpatient cost, a | $300 | $86 | $515 |
| Inpatient cost, b | $24,500 | $3,943 | $45,052 |
| Hospitalization rate, c | 44.30% | 22.0% | 66.0% |
| Case fatality rate, d | 0.20% | 0.2% | 0.2% |
| VSL, e | $9,400,000 | $4,300,000 | $14,200,000 |
| Total cost per case (b × c + a × (1 − c) + d × e) | $29,821 | $9,535 | $58,309 |
The estimated number of measles cases that will occur in contacts exposed during travel (3.6 to 10.1) can be multiplied by the probability of an outbreak with 3 or more cases (12.4% to 21.7%) to estimate the expected number of outbreaks in the absence of public health intervention to conduct contact investigations in exposed travelers. For each outbreak, HHS/CDC assumes that an average of 6 additional cases occur with associated morbidity and mortality costs. The estimated costs of measles outbreaks in the absence of contact investigations for exposed travelers is presented in Table 32.
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| Estimated number of measles cases among contacts, a | 6.85 | 3.6 | 10.1 |
| Probability of measles outbreak, b | 17% | 12.4% | 21.9% |
| Number of additional cases per outbreak, c | 6 | 6 | 6 |
| Estimated number of outbreaks, d = a × b | 1.18 | 0.45 | 2.22 |
| Estimated number of outbreak cases, e = a × b × c | 7.06 | 2.68 | 13.29 |
| Estimated health department costs per outbreak, f | $250,000 | $250,000 | $250,000 |
| Estimated health department costs, g = f × d | $293,989 | $111,607 | $553,758 |
| Average cost per case, h | $29,821 | $9,535 | $58,309 |
| Estimated illness costs, I = h × e | $210,406 | $25,539 | $774,944 |
| Estimated total costs, g + i | $504,395 | $137,146 | $1,328,703 |
HHS/CDC has not received any reports of large measles outbreaks associated with measles cases in patients exposed during travel and contacted by state or local public health departments. As a result, HHS/CDC believes that when measles cases occur in contacts reached by health departments, the probability of an outbreak is significantly mitigated by pre-warning of exposure before disease outset. Given that HHS/CDC estimates that health departments are able to reach approximately 75% of contacts under the status quo, HHS/CDC assumes that the risk of an outbreak has been reduced by at least 60% under the status quo. Further, HHS/CDC assumes that the provisions in the NPRM further improve health departments’ ability to prevent measles outbreaks in cases that occur among travelers exposed during flights. A modest improvement of 15% is assumed (range 10%-20%) resulting in estimated benefits of about $45,000 ($8,000 to $159,000) in Table 33.
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| Estimated total costs without intervention, j = g + i | $504,395 | $137,146 | $1,328,703 |
| Estimated effectiveness of outbreak prevention baseline, k | 60% | 60% | 60% |
| Estimated cost of measles outbreaks under baseline, j × (1 − k) | $201,758 | $54,858 | $531,481 |
| Estimated effectiveness of outbreak prevention with NPRM, l | 69% | 66% | 72% |
| Estimated cost of measles outbreaks with NPRM, m = j × (1 − l) | $156,363 | $46,630 | $372,037 |
| Estimated benefit associated with NPRM, n = j − m | $45,396 | $8,229 | $159,444 |
Alternatives—Measles Contact Investigations
For this analysis, under the less restrictive alternative, HHS/CDC assumes that no contact investigations are performed for measles. As a result, the probability of onward transmission from 3.6 to 10.1 measles patients exposed each year during travel greatly increases and is modeled based on the estimated costs of measles in the absence of intervention $504,000 (range: $137,000 to $1.3 million) (Table 33). Measles outcomes for the more restrictive alternative are the same as estimated for the NPRM since there is no difference in measles efforts between the NPRM and the more restrictive alternative. The comparative benefits relative to the status quo baseline are shown in Table 34. For the less restrictive alternative, costs are estimated based on an increase in measles outbreak costs relative to the baseline.
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| a For the less restrictive alternative, contact investigations are not performed so the cost can be estimated based on the estimated public health benefit of contact investigations performed under the baseline. | |||
| Benefits | |||
| NPRM | $45,396 | $8,229 | $159,444 |
| Less Restrictive Alternative | 0 | 0 | 0 |
| More Restrictive Alternative | 45,396 | 8,229 | 159,444 |
| Costs | |||
| NPRM | 1,950 | 1,950 | 1,950 |
| Less Restrictive Alternative a | 201,758 | 54,858 | 531,481 |
| More Restrictive Alternative | 1,950 | 1,950 | 1,950 |
Effects on Tuberculosis Investigations
The expected benefits associated with reduced tuberculosis morbidity and mortality of contact investigations for exposed travelers are based on a previous analysis, which estimated a return on investment of $1.01 to $3.20 for the baseline situation in which an estimated 19% of exposed contacts are found to have latent tuberculosis infection. [77]The contact rate for exposed tuberculosis contacts is probably higher than for measles because the vast majority of tuberculosis contacts are exposed during international travel as exposed to measles contacts, which are approximately evenly divided between interstate and international travel.
The estimated costs for provide testing and treatment to contacts that test positive for latent tuberculosis infection are estimated to be $1,044 for infected contacts that complete a full course of treatment and $591 for infected contacts that discontinue treatment after 30 days. [78]Following the assumptions in the article, an estimated 28% of persons who test positive for latent tuberculosis infection do not start treatment. An estimated 46% start and complete treatment and the remaining 26% start, but do not complete treatment. The authors estimated that the risk of progression to active tuberculosis is reduced by 80% for those that complete treatment. The authors assumed that there is no effect for individuals that start, but do not complete treatment. HHS/CDC assumes that under the status quo that health departments are able to contact 75% of exposed travelers (based on the reported outcomes from measles contact investigations). [79]
The costs to provide treatment for latent tuberculosis infections under the status quo are summarized in Table 35. In total, the costs are almost $900,000 including about $720,000 to locate contacts and about $180,000 to provide treatment to individuals with latent tuberculosis infection.
| Number of contacts | Estimated cost per contact | Estimated cost | Notes | |
|---|---|---|---|---|
| Estimated cost of contact investigations | 1,995 | $360 | $718,092 | Number of contacts from Table 27 and cost per contact from Table 20. |
| Estimated number of contacts reached by health departments (75%) | 1,496 | NA | Estimated at 75% similar to measles from Table 28. | |
| Estimated number of contacts reached by health departments and have latent TB infection (19% of 75%) | 284 | NA | Estimated 19% of contacts have LTBI (Table 27). | |
| Number of contacts that never start treatment (28%) | 79.6 | 0 | 0 | 28% of 284 contacts with LTBI. |
| Number of contacts that complete treatment (46%) | 130.8 | 1,044 | 136,506 | 46% of 284 contacts with LTBI. |
| Number of contacts that start, but not compete treatment, (26%) | 73.9 | 591 | 43,677 | 26% of 284 contacts with LTBI. |
| Total cost | 898,275 |
The benefits associated with tuberculosis contact investigations are estimated from a published article, which reported a range of $1.01 to $3.20. This analysis did not include the potential benefits from reduced onward transmission of tuberculosis among averted cases, potentially resulting in a conservative estimate of the return on investment. The formula used to derive estimated benefits from estimate costs and return on investment (ROI) is Estimated Costs × ROI + Estimated Costs. The estimated benefits are $2.6 million and are shown in Table 36 (range: $1.8 million to $3.8 million).
| Best estimate | Lower bound | Upper bound | Notes | |
|---|---|---|---|---|
| Estimate costs for contact investigations and treatment | $898,260 | $898,260 | $898,260 | Table 35. |
| Return on investment from tuberculosis contact investigations | 1.91 | 1.01 | 3.20 | Coleman et al. |
| Estimated benefits | 2,613,936 | 1,805,502 | 3,772,691 | = Cost × ROI + Costs. |
The provisions in the NPRM should result in a small increase (assumed 5-15%) in the number of contacts reached by health departments and offered treatment for latent tuberculosis infection. The estimated costs associated with this marginal improvement to reach more contacts can be estimated by multiplying the costs of providing latent tuberculosis ($180,000) by this range of improvement (5%-15%) as shown in Table 37. This results in marginal increased cost associated with NPRM of $18,000 (range: $9,000 to $27,000). The estimated benefits (Table 37) associated the NPRM are $52,000 (range: $18,000 to $114,000).
| Best estimate | Lower bound | Upper bound | Notes | |
|---|---|---|---|---|
| Baseline contact investigation costs | $718,080 | $718,080 | $718,080 | |
| Baseline latent tuberculosis treatment costs | 180,180 | 180,180 | 180,180 | Table 35 costs for latent tuberculosis treatment and testing. |
| Estimated improvement in health departments’ abilities to contact exposed travelers | 10% | 5% | 15% | Assumed. |
| Estimated increased cost for latent tuberculosis treatment under NPRM | 18,018 | 9,009 | 27,027 | Estimated cost for improvement in contact rate as result of NPRM. |
| Estimated costs under NPRM | 916,278 | 907,269 | 925,287 | Estimated baseline cost + increased cost as result of NPRM. |
| Estimated ROI | 1.91 | 1.01 | 3.20 | Table 35. |
| Estimated benefits for NPRM | 2,666,368 | 1,823,610 | 3,886,204 | = Cost × ROI + Costs. |
| Estimated costs associated with NPRM | 18,018 | 9,009 | 27,027 | Calculated from the difference in costs for the NPRM—Baseline costs. |
| Estimated benefits associated with NPRM | 52,432 | 18,108 | 113,513 | Calculated from the difference in benefits for the NPRM − Baseline benefits. |
Alternatives—Tuberculosis Contact Investigations
Under the less restrictive alternative, tuberculosis contact investigation are no longer conducted for persons exposed during travel. Relative to the baseline, there are neither costs to conduct such investigations (resulting in benefits of about $180,000 to forego providing treatment for latent tuberculosis treatment) or benefits associated with reduced tuberculosis morbidity and mortality. Relative to the baseline, the estimated cost of increased tuberculosis morbidity and mortality is estimated to be $2.6 million (range: $1.8 million to $3.8 million). Under the more restrictive alternative in which suspension of entry is enforced in response to quarantinable communicable disease outbreaks, there is no change relative to the NPRM results because it is unlikely that a tuberculosis outbreak would cause suspension of entry. Results are summarized in Table 38.
| Best estimate | Lower bound | Upper bound | Notes | |
|---|---|---|---|---|
| Benefits | ||||
| NPRM | $52,432 | $18,108 | $113,513 | Table 37. |
| Less Restrictive Alternative | 180,180 | 180,180 | 180,180 | Assumed to be the cost to provide LTBI treatment under the baseline (Table 37). |
| More Restrictive Alternative | 52,432 | 18,108 | 113,513 | The more restrictive alternative has the same effect on TB contact investigations as NPRM. |
| Costs | ||||
| NPRM | 18,018 | 9,009 | 27,027 | Table 37. |
| Less Restrictive Alternative | 2,613,936 | 1,805,502 | 3,772,691 | Estimated based on the benefits of avoided TB morbidity and mortality resulting from contact investigations under the baseline. |
| More Restrictive Alternative | 18,018 | 9,009 | 27,027 | The more restrictive alternative has the same effect on TB contact investigations as NPRM. |
Total Costs and Benefits for Measles and Tuberculosis Contact Investigations
The total costs for measles and tuberculosis contact investigation activities are estimated by summing the costs and benefits of measles contact investigations (Table 34) and tuberculosis contact investigations (Table 38). The results are summarized in Table 39.
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| Note: This table includes the sum of results in Tables 34 and 38. | |||
| Benefits | |||
| NPRM | $97,828 | $26,337 | $272,958 |
| Less Restrictive Alternative | 180,180 | 180,180 | 180,180 |
| More Restrictive Alternative | 97,828 | 26,337 | 272,958 |
| Costs | |||
| NPRM | 19,968 | 10,959 | 28,977 |
| Less Restrictive Alternative | 2,815,694 | 1,860,360 | 4,304,172 |
| More Restrictive Alternative | 19,968 | 10,959 | 28,977 |
Total Annual Benefits Resulting from Codification of traveler data collection (71.4 and 71.5) and Change to Definition of “Ill Person” (70.1 and 71.1) Leading to Improved Contact Investigations and Health Outcomes for Measles and Tuberculosis.
The total quantified benefits (Table 40) resulting from the improvement of the quality and timeliness of traveler contact data or the improvement of illness reporting is summarized by summing the improved efficiency for HHS/CDC to provide contact data to health departments and improved efficiency for health departments to contact exposed travelers (Table 23) and the reductions associated with measles and tuberculosis morbidity and mortality (Table 39).
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| Benefits | |||
| NPRM | $117,376 | $26,337 | $312,054 |
| Less Restrictive Alternative | 1,670,940 | 1,670,940 | 1,670,940 |
| More Restrictive Alternative | 176,056 | 85,017 | 370,734 |
| Costs | |||
| NPRM | $19,968 | $10,959 | $28,977 |
| Less Restrictive Alternative | 2,815,694 | 1,860,360 | 4,304,172 |
| More Restrictive Alternative | 19,968 | 10,959 | 28,977 |
The benefits and costs associated with improved effectiveness of contact investigations (Table 40) can be combined with the increased costs to airlines, vessel operators, DOT/FAA, and HHS/CDC to submit and respond to illness reports or to provide more timely and complete traveler contact data for manifest requests (Table 19) to estimate the total annual costs and benefits of the NPRM and for the less restrictive and more restrictive alternatives (Table 41).
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| Benefits | |||
| NPRM | $117,376 | $26,337 | $312,054 |
| Less Restrictive Alternative | 1,777,179 | 1,777,179 | 1,777,179 |
| More Restrictive Alternative | 177,954 | 86,915 | 372,632 |
| Costs | |||
| NPRM | 35,785 | 10,959 | 65,644 |
| Less Restrictive Alternative | 2,815,694 | 1,860,360 | 4,304,172 |
| More Restrictive Alternative | 36,317 | 11,807 | 65,860 |
Other Diseases (Besides Measles and Tuberculosis)
HHS/CDC does not have sufficient data to quantify the health impact of contact investigations for pertussis, rubella, varicella (vessels only), viral hemorrhagic fevers (including Ebola), MERS, or SARS. HHS/CDC does attempt to continuously update its contact investigation protocols based on available evidence. In the past few years, HHS/CDC has stopped requesting data to conduct mumps contact investigations [80] and has modified its protocol to reduce the number of tuberculosis contact investigations. [81]
Experience from interstate flight contact investigations suggest that travelers want to know when they have been exposed to communicable diseases during flights. The first Ebola contact investigation conducted in the United States in October, 2014, found that 60 travelers out of 164 had no contact information on the manifest that was provided by the airline. After an all-night effort by CBP’s National Targeting Center, there were still 24 travelers with no contact information. A second request was made to the airline after it was announced to the media that the airline had contacted over 800 travelers, including travelers who had flown on the same plane subsequent to the flight with the Ebola. At that time the airline was able to provide HHS/CDC more complete information for all travelers. On a second flight, no contact information was provided to HHS/CDC for 111/132 travelers. HHS/CDC again had to request significant assistance from the National Targeting Center to obtain additional contact information. Despite 24 staff-hours spent searching, 28 travelers did not have sufficient information to be able to locate them. HHS/CDC released the flight information in order to inform the public in the hope that the remaining travelers would contact CDC.
It is likely that the need for CDC to put out media requests for travelers to contact the Agency created a level of fear in the general population that may not have been necessary if better contact data were available. In addition, this fear may have led to non-health costs (such as fear of airplane travel) that would have been mitigated if the Agency were able to contact all passengers without the media request. HHS/CDC would like to solicit public comment about potential public willingness to pay to be contacted in the event of exposure to a communicable disease during travel to help estimate the potential benefit to the public of HHS/CDC efforts to work with health departments to contact travelers exposed to meningitis, viral hemorrhagic fevers (including MERS or SARS) among other diseases.
In summary, improved alignment between regulatory text and HHS/CDC’s publicly available guidance should reduce compliance costs for airlines and vessel operators while improving HHS/CDC’s ability to respond to public health threats associated with international and interstate travel. To the extent that airlines and vessel operators improve responsiveness to HHS/CDC traveler data requests, HHS/CDC may become better able to respond to infectious diseases threats and (1) reduce case-loads during infectious disease outbreaks, (2) reduce public anxiety during disease outbreaks, (3) mitigate economic impacts on businesses as a consequence of reduced public anxiety, and 4) reduce the amount of personnel labor time to conduct large-scale CIs in response to a new infectious disease or one with serious public health and medical consequences like Ebola .
Codification of Current Practice (Multiple Provisions in NPRM)
HHS/CDC does not expect that most of the provisions included in the NPRM will result in measurable changes relative to the economic baseline. The primary purpose of the provisions summarized in list below is to elucidate how HHS/CDC interprets its current statutory and regulatory authority under the Public Health Service Act and 42 CFR 70 and 71 regulations. HHS/CDC is grouping the mirror provisions in 70 and 71 in the list below, when they align, to facilitate public review of the current and proposed provisions. These changes are not intended to provide HHS/CDC with new regulatory authorities, but rather to clarify the agency’s standard operating procedures and policies, and due process rights for individuals. HHS/CDC believes that such clarity is an important qualitative benefit of the provisions proposed this NPRM, but is not able to monetize this impact in a robust way.
- Proposed Provisions: § 70.5 Requirements relating to travelers under a Federal order of isolation, quarantine, or conditional release.
○ Baseline and Current Regulatory Provision: § 70.5 Certain communicable disease; special requirements.
Without the NPRM, HHS/CDC may issue Federal orders to restrict travel for persons infected or exposed to quarantinable communicable diseases. However, this process is less transparent and efficient than allowing travel (i.e. issue travel permits to allow interstate travel to persons under Federal orders for diseases not currently identified under existing 42 CFR 70.5.) Under current practice, HHS/CDC issues approximately one Federal order per year, most frequently for tuberculosis, which is a disease not included in the current 70.5.
○ Change relative to baseline as result of NPRM
With the NPRM, HHS/CDC is proposing to align the list of diseases for which individuals under Federal orders may be allowed to travel with the quarantinable communicable diseases specified in Executive Order. A potential future qualitative benefit would be to reduce uncertainty by the individual subject to the order, carrier operators, and cooperating health and law enforcement entities about whether HHS/CDC could issue a travel permit to an individual under a Federal order and quantifiable benefit would be the avoided cost of potential legal challenge.
○ Qualitative benefit/cost of NPRM
Improved transparency for HHS/CDC’s ability to allow individuals under Federal orders to issue travel permits to allow individuals to travel (interstate). HHS/CDC may allow persons under Federal orders to travel interstate for whom there is greater uncertainty regarding HHS/CDC restricting their travel.
○ Monetized benefit/cost of NPRM
Increased clarity around due process may result in fewer resources and time expended by individuals under orders and HHS/CDC in disagreements over HHS/CDC’s authority to issue Federal public health orders that limit an individual’s movement. This includes the potential costs of litigation and associated activities.
- Proposed provisions: § 70.6 Apprehension and detention of persons with specific diseases; § 71.32 Persons, carriers, and things (no change to title)
○ Baseline and Current Regulatory Provision:
Under § 70.6 Apprehension and detention of persons with specific diseases and § 71.32 Persons, carriers, and things HHS/CDC currently has regulatory authority to apprehend and detain individuals with quarantinable communicable diseases.
○ Change relative to baseline as result of NPRM
As a result of these proposed provisions, the major change would be improved transparency of HHS/CDC’s regulatory authority with regard to the issuance of Federal quarantine, isolation, or conditional release orders of individuals traveling interstate.
○ Qualitative benefit/cost of NPRM
Improved transparency and compliance with Federal orders.
○ Monetized benefit/cost of NPRM
Increased clarity around due process may result in fewer resources and time expended by individuals under orders, cooperating entities, and CDC in disagreements over HHS/CDC’s authority to issue Federal public health orders that limit an individual’s movement. This includes the potential costs of litigation and associated activities.
- Proposed Provisions: § 70.10 Public health prevention measures to detect communicable disease; § 71.20 Public health prevention measures to detect communicable disease.
○ Baseline and Current Regulatory Provisions: No explicit regulatory provision.
In the absence of the NPRM and under existing statutory authority provided in the Public Health Service Act, HHS/CDC could still implement public health measures at locations where individuals may gather for interstate travel or at U.S. ports of entry. However, without concrete regulatory authority to require such measures, travelers may not comply, either by refusing to answer risk assessment questions or providing false information. This lack of compliance may require that HHS/CDC, if it reasonably believes that the individual is infected with or has been exposed to a quarantinable communicable disease, to quarantine, isolate, or place the individual under surveillance under 42 CFR 71.32 and 71.33. HHS/CDC has not implemented public health measures at locations where individuals may congregate for the purposes of interstate travel in at least 50 years and cannot predict if or how often it may implement measures in the future.
○ Change relative to baseline as result of NPRM
Improved transparency and potentially improved compliance in the event that HHS/CDC implements such measures in the future.
○ Qualitative benefit/cost of NPRM
Improved transparency and public understanding of HHS/CDC’s rationale and authority to conduct such measures and require individuals to comply.
○ Monetized benefit/cost of NPRM
Increased clarity around due process may result in fewer resources and time expended by individuals under orders and HHS/CDC in disagreements over HHS/CDC’s authority to issue Federal public health orders that limit an individual’s movement. This includes the potential costs of litigation and associated activities.
- Proposed Provisions: § 70.12 Medical examinations; § 71.36 Medical Examinations
○ Baseline and Current Regulatory Provisions: 71.33 Persons: Isolation and Surveillance.
This is carried out under statutory authority and under the regulatory authorities in 42 CFR 71.33 Persons: Isolation and surveillance, which have been interpreted to allow for medical examinations of individuals under Federal orders.
○ Change to baseline as result of NPRM
With the NPRM, the major change would be an alignment between the statutory language in the Public Health Service Act and improved transparency of HHS/CDC’s regulatory authority.
○ Qualitative benefit/cost of NPRM
Improved transparency and public understanding of HHS/CDC’s rationale and authority to conduct such measures and require individuals to comply.
○ Monetized benefit/cost of NPRM
Increased clarity around due process may result in fewer resources and time expended by individuals under orders, cooperating entities, and HHS/CDC in disagreements over HHS/CDC’s authority to issue Federal public health orders that limit an individual’s movement. This includes the potential costs of litigation and associated activities.
- Proposed Provisions: § 70.14 Requirements relating to the issuance of a Federal order for quarantine, isolation, or conditional release; § 71.37 Requirements relating to the issuance of a Federal order for quarantine, isolation, or conditional release
○ Baseline and Current Regulatory Provisions: No current explicit regulatory provision
Without the NPRM, HHS/CDC can under current statutory provided by the Public Health Service Act and regulatory authority continue to issue Federal quarantine, isolation, or condition release orders. However, the process executed under statutory authority and internal policy and standard operating procedures derived from regulations at42 CFR 71.32 Persons, carriers, and things and 71.33 Persons: Isolation and Surveillance, which is not as transparent to the public as an explicit regulation outlining requirements.
○ Change to baseline as result of NPRM
Improved transparency around HHS/CDC’s authority for, and requirements and processes related to, the issuance of Federal quarantine, isolation, and conditional release orders.
○ Qualitative benefit/cost of NPRM
Improved transparency and public knowledge of HHS/CDC’s procedures and regulatory requirements.
○ Monetized benefit/cost of NPRM
None. This is a clarification of HHS/CDC’s current practice.
- Proposed Provisions: § 70.15 Mandatory reassessment of a Federal order for quarantine, isolation, or conditional release; § 71.38 Mandatory reassessment of a Federal order for quarantine, isolation, or conditional release
○ Baseline and Current Regulatory Provisions: No current explicit regulatory provision.
Without the NPRM, HHS/CDC can under current statutory authority provided by the Public Health Service Act and regulatory authority under 42 CFR 71.32 Persons, carriers, and things and 71.33 Persons: Isolation and Surveillance continue to issue Federal quarantine, isolation, or condition release orders. However, the process for a reassessment of a Federal order is executed under internal policy and standard operating procedures, which is not as transparent to the public as regulation.
○ Change to baseline as result of NPRM:
With the NPRM, individuals under Federal order may be more aware of mandatory reassessment of a Federal quarantine, isolation, or conditional release order.
○ Qualitative benefit/cost of NPRM
Improved transparency and understanding of due process protections under a Federal public health order.
○ Monetized benefit/cost of NPRM
Increased clarity around due process may result in fewer resources and time expended by individuals under orders and HHS/CDC in disagreements over HHS/CDC’s authority to issue Federal public health orders that limit an individual’s movement. This includes the potential costs of litigation and associated activities.
- Proposed Provisions: § 70.16 Medical review of a Federal order for quarantine, isolation, or conditional release; § 71.39 Medical review of a Federal order for quarantine, isolation, or conditional release
○ Baseline and Current Regulatory Provisions: No current explicit regulatory provision.
Without the NPRM, HHS/CDC can under current statutory authority provided by the Public Health Service Act and regulatory authority under 42 CFR 71.32 Persons, carriers, and things and 71.33 Persons: Isolation and Surveillance continue to issue Federal quarantine, isolation, or condition release orders. However, the process for a medical review of a Federal order is executed under internal policy and standard operating procedures, which is not as transparent to the public as regulation.
○ Change to baseline as result of NPRM:
With the NPRM, individuals under Federal order may become aware of their right to a medical review, and exercise that right, under this due process provision.
○ Qualitative benefit/cost of NPRM
Improved transparency and understanding of due process afforded to individuals under a Federal order
○ Monetized benefit/cost of NPRM
Increased clarity around due process may result in fewer resources and time expended by individuals under orders and HHS/CDC in disagreements over HHS/CDC’s authority to issue Federal public health orders that limit an individual’s movement. This includes the potential costs of litigation and associated activities.
- Proposed Provisions: § 70.17 Administrative records relating to Federal quarantine, isolation, or conditional release; § 71.29 Administrative records relating to Federal quarantine, isolation, or conditional release
○ Baseline and Current Regulatory Provisions: No current explicit regulatory provision.
Without the NPRM, HHS/CDC can issue under current statutory provided by the Public Health Service Act and regulatory authority under 42 CFR 71.32 Persons, carriers, and things and 71.33 Persons: Isolation and Surveillance continue to issue Federal quarantine, isolation, or condition release orders. However, the process and requirement for documentation for the administrative record is executed under statutory authority, internal policy and standard operating procedures, which is not as transparent to the public as regulation.
○ Change to baseline as result of NPRM
The requirement, with which HHS/CDC is already complying, will clarify for the public that certain documents must be retained for the administrative record.
○ Qualitative benefit/cost of NPRM
Improved transparency
○ Monetized benefit/cost of NPRM
Not applicable. This is a codification of an administrative activity within HHS/CDC.
- Proposed Provisions: § 70.18 Agreements; § 71.40 Agreements
○ Baseline and Current Regulatory Provisions: No current explicit regulatory provision.
Without the NPRM, individuals may not be aware of the agreement process. HHS/CDC can under current statutory and regulatory authority continue to issue Federal quarantine, isolation, or condition release orders. However, the process and requirement for documentation for the consent process is executed under statutory authority, internal policy and standard operating procedures, which is not as transparent to the public as regulation.
○ Change to baseline as result of NPRM
With the NPRM, individuals are more likely to be aware of the agreement process.
○ Qualitative benefit/cost of NPRM
Improved transparency
○ Monetized benefit/cost of NPRM
Increased clarity around due process may result in fewer resources and time expended by individuals under orders, cooperating entities, and HHS/CDC in disagreements over HHS/CDC’s authority to issue Federal public health orders that limit an individual’s movement. This includes the potential costs of litigation and associated activities.
- Proposed Provisions: § 70.19 Penalties/§ 71.2 Penalties
○ Baseline and Current Regulatory Provision: § 71.2 Penalties. Part 70 currently has no penalties provision.
Without the NRPM, individuals may not be aware of the increase in the maximum allowable penalties for a violation of regulations under 42 CFR 70 and 71. And it may not be clear to individuals that a violation of quarantine regulation found in 42 CFR part 70 may result in penalties.
○ Change to baseline as result of NPRM
With the NRPM, there will be less confusion about the maximum allowable penalties for a violation of regulations under 42 CFR 70 and 71.
○ Qualitative benefit/cost of NPRM
Improved transparency and alignment with current law under 18 U.S.C. 3559 and 3571.
○ Monetized benefit/cost of NPRM
No individual has been issued a penalty under this regulation, so monetizing this benefit or cost is not feasible. This is simply an effort to align the domestic and foreign quarantine penalties provisions, and updates outdated regulatory language so that it reflects current statutory language concerning criminal penalties.
The 2014-2016 Ebola Outbreak
The costs and benefits from the 2014-2016 Ebola enhanced entry risk assessment and management program are used to demonstrate the costs and benefits of implementation of its regulatory authorities, and are especially relevant when analyzing the effects of the rule relative to a non-status quo baseline. Although most of the costs incurred by HHS/CDC, DHS/CBP, and travelers can be quantified, the benefits are more difficult to quantify. This program is chosen because of its significant economic impacts. For this outbreak analysis, a less restrictive alternative would be for HHS/CDC not to execute its existing regulatory authorities to implement the Ebola enhanced entry risk assessment and management program. The more restrictive alternative would be a suspension of entry for persons from countries with widespread transmission for a period of 21 days (equivalent the maximum expected incubation period for Ebola disease).
The quantified cost of the Ebola enhanced entry risk assessment and management program ($109 million) outweighs what HHS/CDC estimates as directly associated-benefits ($7.7 million), but there are multiple benefits that HHS/CDC could not estimate. Around the time the program was implemented, public opinion surveys ranked Ebola as the third highest health care concern among a list of issues facing the country, only health care costs and access to care ranked higher. The same poll found that about 45% were either somewhat worried or very worried that they or someone in their family could become sick with Ebola. The Ebola enhanced entry risk assessment and management program in combination with a number of other Federally-funded initiatives helped reduce the potential risk for Ebola exposure in the United States from travelers from the affected countries to almost zero.[82] The average cost per American citizen for these programs was approximately $17. Thus, if willingness to pay for such a risk reduction was greater than $17 per person on average, the programs would pass a cost-benefit test. Finally HHS/CDC examined the economic impact of the recent MERS outbreak in South Korea and asks the question, what would be the cost to the United States if an outbreak of similar magnitude occurred. HHS/CDC estimates the cost of such an outbreak could be as much as $58 billion indicating the potential costs associated with unexpected outbreaks of quarantinable communicable diseases.
In late 2014, two imported cases of Ebola were identified in the United States, one of which resulted in two domestic cases and extensive contact investigations in the community and for travelers on two domestic flights. 83 84 85 86
Around the same time, some political leaders and members of the public demanded increasing the domestic response, including banning air travel between the United States and the three countries with widespread transmission. [87] Many public health professionals cautioned that such a ban would cause greater harm than good to the public health response by hampering travel of responders and delivery of supplies into the region and paradoxically could increase the risk for spread via covert and circuitous travel routes. 88 89 The paradox results because travel restrictions cannot stop people from moving across borders and spreading disease to new countries, especially because such travel is often more difficult to track than if travel is not restricted entirely. [90]
To reduce the risk of importation of Ebola to the United States, HHS/CDC supported the implementation of exit screening at international airports in countries with widespread Ebola transmission. After Ebola spread from Liberia to Nigeria by air travel, concerned airlines canceled flights to Guinea, Liberia, and Sierra Leone, and multiple countries closed their borders to travelers from these countries; [91] the shortage of commercial flights caused delays to the provision of humanitarian aid, resulting in shortages of medical supplies, personal protective equipment, and food. [92] The few airlines that continued to fly to the countries with Ebola outbreaks insisted that departing travelers be screened before boarding. [93] HHS/CDC Border Health teams in Guinea, Liberia, Nigeria, and Sierra Leone, and later Mali and Senegal, helped airport and health authorities implement airport exit screening measures that included administering an exposure-and-symptom questionnaire and at least one temperature check with a handheld noncontact thermometer to all departing passengers. Health screeners were trained to conduct secondary assessments of travelers who reported possible exposures or who had symptoms compatible with Ebola. Symptomatic or exposed travelers were denied boarding and referred for further medical and public health assessment. As national databases of known contacts became more robust, they were matched against passenger manifests for departing flights. These measures helped countries with Ebola outbreaks meet WHO recommendations and ensured that some commercial air carriers continued to fly to these countries, serving as vital conduits for supplies and response personnel.
During August 2014-January 2016, approximately 300,000 travelers were screened in Guinea, Liberia, and Sierra Leone. Only four cases of Ebola were exported through air travel to other countries (United States [two cases], United Kingdom [one case], Italy [one case]) after exit screening was implemented; none of the infected travelers were overtly symptomatic at the time of travel. 94 95 96 97 No Ebola cases were reported to have been detected during exit screening.
To build on the exit screening already in place, HHS/CDC collaborated with the U.S. Department of Homeland Security to initiate an enhanced entry risk assessment and management program for travelers from countries with Ebola outbreaks. This unprecedented operation required coordination across multiple U.S. government agencies, as well as with airport authorities and health departments in all U.S. states and territories. [98]
HHS/CDC issued revised interim guidance in October 2014 [99] after the first imported case of Ebola in the United States was identified (and initially diagnosed as presumed sinusitis) in Dallas, Texas; [100] an infected U.S. health care worker (HCW) flew on two domestic commercial flights, causing panic among U.S. travelers and disrupting the travel industry; 101 102 103 and an infected humanitarian aid worker was reported to have been in public areas, including the New York City subway, during the early stages of his illness. 104 105 CDC’s guidance was revised in response to assertions that self-monitoring was insufficient; growing concerns about infected HCWs in Spain, the United States, and the West African countries with Ebola outbreaks;106 107 108 109 and renewed calls for travel bans. [110] Demands to restrict movement of HCWs caring for patients with Ebola were countered by predictions that stringent restrictions would discourage HCWs from supporting the response in West Africa or taking care of patients with Ebola at designated facilities in the United States. 111 112 The revised guidance recommended that state or local public health authorities assume responsibility for monitoring all potentially exposed persons for the duration of the 21-day incubation period (active monitoring); established a higher standard of monitoring (direct active monitoring that included daily direct observation by public health officials) for persons with greater potential risk for exposure, including HCWs; and provided guidance for possible application of movement restrictions within communities. Although CDC’s guidance represented a minimum standard, states could, and in many cases did, apply more restrictive measures (e.g., temporarily quarantining HCWs returning from West Africa). [113] Many of these measures were enacted before CDC issued the updated guidance.
Objectives of the Enhanced Entry Risk Assessment Process
Enhanced entry risk assessment had three main objectives:
- To identify travelers who may have been exposed to Ebola, or be sick when they arrive in the United States,
- To ensure that these travelers were directed to appropriate care and monitoring, if needed, which would also help protect the health of all Americans, and
- To educate travelers and provide tools to help them monitor themselves for symptoms, and report to the local or state health department at their domestic destination(s) for active monitoring and health care if they developed symptoms.
Beginning October 2014, all travelers from Guinea, Sierra Leone and Liberia were required to undergo risk assessment for Ebola. Enhanced entry risk assessment was discontinued for countries after widespread transmission of Ebola had been halted. The last travelers from Guinea were screened in February 2016. Enhanced entry risk assessment at U.S. airports included processes (referred to operationally as “primary screening”) to identify travelers from countries with Ebola outbreaks, either through scheduled flight itineraries or during customs and immigration inspections. CBP officers and other U.S. Department of Homeland Security staff collected contact and locating information, administered an exposure-and-symptom questionnaire, checked travelers’ temperatures with noncontact thermometers, and observed travelers for signs of illness. Data were entered electronically through an online interface and transmitted securely to a CDC database and then to states. These processes were collectively referred to as “secondary screening.” Travelers who were symptomatic or who reported possible exposures were referred to CDC for an in-depth public health risk assessment (referred to as “tertiary screening”). Symptomatic travelers who met predefined criteria were referred for medical evaluation to designated assessment hospitals, in consultation with the health department with jurisdiction for the airport. Travelers with certain types of higher risk exposures were not permitted to travel further by commercial transport even if they were not symptomatic.
HHS/CDC developed a new intervention called the CARE (Check and Report Ebola) Program to supplement the Ebola entry screening process. Airport-located CARE `Ambassadors’ that connected with travelers were trained health educators, counselors, or social workers. Each traveler arriving from West Africa was counseled by a CARE Ambassador and received a CARE Kit that included educational materials, a digital thermometer, and a pre-paid cell phone to help with daily reporting to state or local health departments.
Analysis of the Costs of Ebola Enhanced Entry Risk Assessment and Management Program
Every public health emergency is different, but HHS/CDC is confident that had the agency been able to answer `who, where and how,’ the government expenditures on Ebola entry risk assessment program would have been lower. In the absence of such data, HHS/CDC had to implement an expensive program in part just to help identify the small number of people within the United States that had been in countries with widespread Ebola transmission within the previous 21 days.
While some HHS/CDC and CBP personnel would still undoubtedly have been assigned to airports, some costs associated with travel time, training, and airport Ebola response work may have been avoided with the availability of better traveler contact data. More specifically, some examples cutting back on the domestic response might include:
- Reduction in travel of HHS/CDC employees assigned to airports. Each reassigned employee receives airfare, hotel, and per diem for incidentals such as meals.
- Reduction in overtime. Initially, staff at airports universally worked seven days a week, 12 to 16 hours a day, for 30 days at a time. At HHS/CDC headquarters, the Emergency Operations Center had persons answering calls 24-7, and many others working seven days to make travel arrangements, provide supplies, and answer press or congressional inquiries. Middle- and upper-level managers in more than one CDC center and division, as well as the HHS/CDC Director and staff, were on call 24-7.
- Reduction in supplies. The people reporting to airports needed personal protective gear, cellphones, laptops, and phones. At different points in time during the response, some airports needed to supply special contractors to remove used protective gear.
During the past fifteen years there have been several international disease events where this type of risk assessment was either considered by HHS/CDC or suggested by other branches of Federal government,e.g., SARS, MERS, and multiple novel influenzas. However, this was the first instance in which such a program was implemented.
Ebola Entry Risk Assessment Cost Estimates
First this section estimates the time-costs or opportunity costs to travelers from West Africa to comply with protocols at the ports of entry. Then HHS/CDC provides estimates of the budgetary costs to HHS/CDC and CBP for standing up the Ebola entry risk assessment program.
Screened-Traveler Opportunity and Out-of-Pocket Costs
The actual number of travelers who underwent the risk assessment program at airports between October 11, 2014 and February 18, 2016 is summarized in Table 42. These numbers were tabulated using electronic records kept by HHS/CDC of the number of West African travelers screened at U.S. airports.
Using the numbers of travelers screened, HHS/CDC estimates the opportunity costs for travelers. To represent the time involved in waiting for, and complying with, risk assessment for travelers, HHS/CDC assumes 30 minutes per traveler for secondary screening and an additional 30 minutes for travelers that had to undergo tertiary screening. Primary screening time was not included because all international travelers already interact with CBP in order to enter the United States.
Hospital evaluations would require an additional 24 hours. The cost to provide transportation to hospitals from airports and to conduct further evaluation was covered by travelers and/or their insurance providers or employers. Over the 16 month period of this program, a total of 29 travelers out of 38,344 screened (0.08%) were recommended to travel from the airport to a hospital for further testing. All travelers complied voluntarily and there was no need to issue a Federal order. HHS/CDC does not have any data to estimate the cost of transportation to and evaluation at hospitals. The cost to treat Ebola patients was reported to be about $30,000 per day at the Nebraska Medical Center and about $50,000 per day at the National Institutes of Health. [114] If the daily cost of evaluation is estimated to be similar to the cost of treating Ebola patients (i.e. $30,000—$50,000 per day) and it is assumed that evaluation requires 24-48 hours, a lower bound cost estimate for evaluation would be $30,000/day × 1 day = $30,000 and an upper bound cost estimate can be calculated from $50,000/day × 2 days = $100,000. The midpoint cost estimate is $65,000. For 29 patients at the midpoint cost estimate, the total cost is 29 patients × $65,000 per patient = $1,885,000.
During a one-year period from August 2013 through July 2014, approximately 90% of passengers from Liberia, Guinea, and Sierra Leone entered the United States at the five airports that CBP funneled all West African travelers for Ebola risk assessment. Therefore, HHS/CDC assumes that 10% of travelers designated for risk assessment had to change travel plans to comply with the funneling restrictions. This re-routing likely resulted in increased time spent in transit and some unplanned out-of-pocket expenditures for items such as rescheduled flights, layover delays or meals. In the absence of data to quantify these costs, HHS/CDC assumed that re-routing required an additional 6 hours of travel time and a $100 increase in costs for each traveler redirected from their original destination. This would apply to 10% of 38,344 (3,834) travelers over an 18-month period.
Traveler opportunity costs are valued at $23.23 per hour [115] /60 minutes to arrive at an estimate of $0.39 per minute using the 2015 U.S. average hourly wage reported by the Bureau of Labor Statistics. The total opportunity costs for travelers funneled to airports and participating in risk assessment is estimated to be $744,834 and the total out-of-pocket cost is estimated at $2.3 million (including the cost of evaluation at hospitals after referrals from airports. Thus, the total traveler cost is $3,146,596 (Table 42).
| Number of travelers a | Time per traveler (min) | Time cost per traveler-hour b | Total opportunity cost | Out-of-pocket cost c | Total | |
|---|---|---|---|---|---|---|
| a All travelers identified from countries with widespread Ebola transmission. | ||||||
| b Time cost is estimated by multiplying no. of minutes/60 by $23.23 (average hourly wages according to the 2015 Occupation and Employment Survey. | ||||||
| c Assumed $100 per travelers for 10% of travelers that are redirected. | ||||||
| d Secondary and Tertiary Screening | ||||||
| 2nd d | 38,344 | 30 | $23.23 | $445,366 | $0 | $445,366 |
| 3rd d | 2,736 | 30 | 23.23 | 32,867 | 0 | 32,867 |
| Hosp. | 29 | 1,440 | 23.23 | 25,471 | 1,885.000 | 1,910,471 |
| Funnel | 3,834 | 360 | 23.23 | 374,453 | 383,440 | 757,893 |
| Total | 38,344 | NA | NA | 744,834 | 2,268,440 | 3,146,596 |
Federal Government Spending for Ebola Entry Risk Assessment
Current and projected spending for initiation and compliance with Ebola entry risk assessment is about $96M for HHS/CDC. All HHS/CDC funds have been either spent or are obligated in Fiscal Year (FY) 2016. CBP spending as of May 18, 2015 was $4.9 M. If this level of spending is extrapolated to 16 months of steady state spending, CBP costs would be $9.8 million. HHS/CDC does not have estimates of the costs to the other Federal or state agencies or airlines for time spent working in conjunction with HHS/CDC staff to develop the domestic response to Ebola.
Although Federal government spending occurred over 16 months, the monies were allocated and obligated within a single calendar year. Thus, the spending amounts are not discounted, but rather are treated as a one-time spending event. The total cost ($109 million) to the U.S. Federal government and to travelers is summarized in Table 43.
| Budget/cost category | Event cost |
|---|---|
| CDC Budget | $96,026,532 |
| CBP Budget | 9,830,583 |
| Passenger Opportunity and Out-of-Pocket Cost | 3,146,596 |
| Total 16 Months | 109,003,711 |
Analysis of the Benefits of Ebola Enhanced Entry Risk Assessment and Management
The benefits of the Ebola enhanced entry risk assessment and management program are much more difficult to quantify than the costs. This program was part of more than $5.4 billion spent on emergency Federal programs in the United States and abroad to contain the Ebola epidemic in West Africa to minimize the risk to the U.S. public.
The potential benefits from the enhanced entry risk assessment and management program include:
- Reduced time to health care evaluation/isolation for cases
- Treatment at appropriate facilities leads to better outcomes, reduced transmission risk
- Quarantine of persons at high risk to prevent transmission
- Reduction in effort by state/local health departments to conduct active monitoring due to increased engagement/communication tools (CARE program)
For the Ebola enhanced entry risk assessment and management program to be effective, there were a number of other activities conducted in parallel. Health departments had to effectively implement active monitoring and quarantine restrictions to respond to travelers who may become ill during the 21-day period in which travelers from Ebola-affected countries could become ill. Available evidence suggests that all states conducted active monitoring at least as stringently as the guidelines circulated by HHS/CDC. In fact, analysis of publicly available state guidelines determined that 17 states and the District of Columbia had policies that were more restrictive than HHS/CDC guidance, 35 states and territories had policies equivalent to HHS/CDC guidance, and no states or territories had guidance that was less restrictive than HHS/CDC guidance. [116] Travelers must comply with monitoring/quarantine and give accurate information during entry risk assessment. Treatment facilities must be able to appropriately evaluate and treat patients. Part of the Federal Ebola funding was used to identify and prepare hospitals to treat Ebola patients. Laboratory testing must be accessible, accurate, and timely to properly diagnose patients with communicable diseases not commonly seen in the United States.
The groups at greatest risk to contract Ebola, MERS, and SARS in non-endemic countries have been health care workers and patients in hospital settings. [117] This points to the importance of infection control processes at hospitals. However, the outcome from the first Ebola patient diagnosed with Ebola after arrival in the United States can be compared to the outcome of the second patient to demonstrate the utility of properly linking persons with potentially devastating communicable disease to treatment at a facility that has prepared to treat such patients. All of the other Ebola cases treated in the United States were diagnosed while the patients were in West Africa and are not included in this analysis.
The first incident case of Ebola in the United States among a traveler exposed in West Africa was diagnosed in a foreign national at a hospital in Dallas, Texas. At the initial presentation, the hospital did not suspect Ebola and did not test the patient before releasing him back into the community. As the patient’s health continued to deteriorate, he returned to the same hospital and was then diagnosed with Ebola. Fortunately, there was no transmission to others in the community during the time between the initial and follow-up visits. During treatment, two health care workers at the hospital contracted Ebola, one of which flew on an interstate flight to and from Cleveland, Ohio. This single case led to 516 contacts who underwent active monitoring by health departments in six states. Among the 516 contacts, 147 were health care workers all of whom were exposed at the first hospital. All 147 health care workers had voluntary movement restrictions and 30 underwent voluntary home quarantine. 118 119 In addition, there were 101 persons exposed in the community and who were actively monitored in Texas and Ohio of which 41 had restricted movement and 9 underwent home quarantine. 120 121 122 Finally, there were 274 travelers exposed during interstate travel and actively monitored in 6 states. Of these, 20 travelers had movement restrictions.[123] In Texas and Ohio, 7 schools were closed for one day, and 2 students were asked not to go to school for 21 days after being on same flight as the infected health care worker. [124]
In contrast, the second incident case of Ebola among a traveler from West Africa in the United States occurred in New York City. However, the patient was a health care worker that volunteered in a treatment center in West Africa. Per CDC guidance, the patient had been self-monitoring his temperature and symptoms. The patient was quickly identified as at risk for Ebola and was transported to a hospital designated to be capable of accepting potential Ebola patients. This patient did not infect any healthcare workers and only 3 community contacts and zero health care workers had movement restrictions imposed. [125] There were no school closures in New York.
A comparison of estimated costs incurred for the first versus second incident cases of Ebola in the United States is presented in Tables 44 and 45. The opportunity costs for health care workers placed under movement restrictions are estimated based on average health care worker salary reported in the 2015 Occupational and Employment Statistics Survey ($37.40 per hour, code 29-0000) assuming that each employee is unable to work for a period of 3 weeks (15 work days). The costs to public health departments are estimated based on the average salary of epidemiologists ($36.97 per hour, code 19-1041) assuming that 50 epidemiologists spent a total of 30 days working on investigations for the three cases originating in Dallas. An overhead multiplier of 100% is used to estimate employee benefits and overhead costs.
Persons placed under movement restrictions are usually not permitted to go to public areas such as grocery stores and pharmacies. In addition, homeless contacts may need to be provided with temporary housing to facilitate active monitoring. [126] Some states posted police officers at specific addresses at an estimated cost of $1,000 per day. [127]The estimated average cost for the services required to monitor and sustain persons with restricted movement is estimated to be $500 per person-day for 21 days. In addition, 7 one-day school closures were reported. HHS/CDC does not have any data on school sizes and assumes that the average school size is 300 students and that opportunity costs of a one-day school closure can be estimated based on a parent or guardian losing one half-day of work (4 hours) for every student. Parent and guardian opportunity costs are estimated using the average wage rate in the United States ($23.23 per hour). [128] The cost to treat an Ebola patient has been reported to be about $650,000 [129] at the Nebraska Medical Center and has been estimated to exceed $1 million. [130] HHS/CDC estimates the treatment cost to be the midpoint of these estimates $825,000 per case). It is not clear if this estimate includes the cost of waste disposal associated with Ebola treatment. The cost of waste disposal has been estimated to be as much as $100,000 per Ebola patient-day. [131] HHS/CDC assumes the cost of waste disposal is not included in the reported treatment costs and that waste disposal over a 10-20 period of treatment would add another $1 million to the cost of treatment. This results in an average cost of treatment and waste disposal of $1.825 million per patient.
| Category | Number | Cost | Notes |
|---|---|---|---|
| Health care workers missing work | 147 | $659,736 | Assume all persons with travel restriction missed time at work/productivity (21 days). |
| Community | 41 | 114,292 | |
| Air travelers | 20 | 55,752 | |
| Restricted movement support costs | 208 | 2,184,000 | Assume support costs for movement restrictions or home quarantine are 500 per person-day for 21 days. |
| Public health response | 50 (assumed) | 887,280 | Assume 50 public health workers worked full time on response for 30 days. |
| School closure | 7 | 195,132 | 7 schools for 1 day, assume 300 students each and one parent lost one half day of productivity per student. |
| Ebola treatment | 3 | 5,475,000 | Assume treatment cost = 1,825,000 per patient. |
| Total | 9,571,192 |
| Category | Number | Cost | Notes |
|---|---|---|---|
| Health care workers missing work | 0 | $0 | Assume all persons with travel restriction missed time at work. |
| Community | 3 | 8,363 | |
| Air travelers | 0 | 0 | |
| Restricted movement support costs | 3 | 31,500 | Assume support costs for movement restrictions or home quarantine are 500 per person-day for 21 days. |
| Public health response | 5 | 62,832 | Assume 5 public health workers worked full time on response for 21 days. |
| School closure | 0 | 0 | |
| Ebola treatment | 1 | 1,825,000 | Assume treatment cost = 1,825,000. |
| Total | 1,927,695 |
The difference ($7.7 million) in total estimated costs associated with the first incident case in a traveler from West Africa ($9.6 million) and the second incident case ($1.9 million) show the potential benefits associated with the Federal, state and local activities implemented to link patients to appropriate care to mitigate the transmission risk. HHS/CDC does not have any more data with which to estimate the costs associated with incident Ebola cases in the United States and solicits public comment to improve the above cost estimates.
At the time the Ebola enhanced entry risk assessment and management program was put in place, HHS/CDC could not accurately estimate the expected number of travelers from West Africa that would become sick with Ebola after arrival in the United States. In retrospect, efforts to contain the transmission of Ebola from countries with widespread transmission were very effective at limiting risk. Among all 300,000 travelers departing countries with widespread transmission via commercial airlines, only four Ebola cases were reported, none of which were symptomatic during travel. Although less than 20% of such travelers were destined for the United States, two of the four cases occurred in the United States.
Public Willingness To Pay for Ebola Prevention Measures
HHS/CDC was unable to conduct a willingness to pay survey to assess the U.S. public’s willingness to expend Federal resources to minimize Ebola risks. However, survey evidence suggests that the public would probably be willing to pay some amount to reduce risk from Ebola to as close to zero as possible. Soon after Ebola was transmitted to two health care workers in the U.S., a poll showed that Americas felt Ebola was an urgent health problem for the entire country. Among a list of health care issues facing the country, only health care costs and access to care ranked higher than Ebola in the public’s mind. In comparison, both heart disease and cancer were ranked below Ebola despite a significantly greater probability that any individual would suffer from these conditions than contract Ebola. [132]
Public opinion related to disease outbreaks can influence policy leader attitudes related to the response of the outbreak—potentially redirecting the focus of activities and public funding to areas of limited public benefit. In a review of over 175 public opinion polls in 2014, researchers highlighted several reasons for this public perception.
Survey respondents did not understand or trust information provided regarding the mode of transmission and therefore they felt particularly vulnerable. About 45% were either somewhat worried or very worried that they or someone in their family could become sick with Ebola. The media also played a role in increasing the public’s concern—three major news networks aired approximately 1000 Ebola-related segments between mid-October to early November, 2014. According to the survey, public trust in scientists and government was at an all-time low. [133]
Considering that the U.S. population as a whole (319 million), an average willingness to pay per person of $17 would be sufficient to justify the entire $5.4 billion Federal Ebola response. This amount would cover the costs of Federal government activities to reduce Ebola transmission in affected countries, to support exit screening at international airports, research programs for Ebola vaccines and medicines, to implement domestic programs to identify and prepare U.S. hospitals and laboratories for Ebola testing and treatment, to implement the Ebola enhanced entry risk assessment and management program at U.S. airports, and to provide Federal support for active monitoring activities in U.S. states. The $5.4 billion budget allocation included $1.147 billion for domestic Ebola response activities (other than research and development) including the $96 million for the Ebola enhanced entry risk assessment and management program. Thus, if international, research, and development activities are excluded, U.S. public willingness to pay would have to be greater than $3.65 per person for all domestic activities or $0.34 for just the enhanced entry risk assessment and management program. HHS/CDC would like to solicit public comment on willingness to pay to reduce Ebola risk in the United States to near zero if another outbreak of Ebola occurs in the future.
Potential for Disease Transmission in the United States
HHS/CDC believes that the risk of significant transmission of Ebola in the United States is low and that Federal, state, and local public health interventions reduced such risks to almost effectively zero. However, as discussed above, outbreaks of new diseases can lead to significant costs if disease-related anxiety leads to reduced productivity. Thanks in part to vigorous Federal responses to communicable disease threats, the United States has never experienced a time-limited introduction of a new communicable disease with significant transmission. This analysis would not apply to a communicable disease threat like the novel H1N1 influenza pandemic that would infect a significant number of U.S. citizen regardless of HHS/CDC efforts. However, other relatively high income countries have had to deal with very costly outbreaks of SARS and MERS.
The 2003 SARS outbreak was initiated in Guandong, China in late 2002 and led to the exportation of cases to multiple countries, including Australia, Canada, Hong Kong, Singapore and the United States. Significant transmission occurred in Hong Kong, Canada, and Singapore. The introduction of SARS led to reductions in the number of people traveling to these countries. Survey respondents indicated that they were less likely to engage in activities such as eating at restaurants or going to shopping malls. Forecasted Gross Domestic Product (GDP) in 2003 decreased by 3.7 billion US dollars in Hong Kong, 3.2-6.4 billion US dollars in Canada, and 4.9 billion US dollars in Singapore due to the SARS outbreak. [134] In Canada and Singapore, GDP growth was estimated to decrease by 1% for the year 2003. In the second quarter of 2003, GDP growth in China and Hong Kong was estimated to have decreased by 3% and 4.75%, respectively. [135] The estimated losses to the tourism industry alone in Beijing, China was around 1.4 billion US dollars. [136]
The MERS outbreak in South Korea started with a case in an international traveler returning from the Middle East at the end of May 2015 and ended with the official announcement of the World Health Organization in December 2015. A total of 186 laboratory-confirmed infections, including 38 deaths, was reported, and more than 16,000 people kept in-house quarantine. [137] This outbreak represents an infectious disease outbreak associated with international travel in a high income country. Since this outbreak recently occurred in 2015, it may provide a useful extrapolation of what might happen if HHS/CDC does not act swiftly to contain a quarantinable communicable disease threat.
HHS/CDC assumes an outbreak similar in magnitude to the Korean MERS outbreak is more likely to happen in the United States if HHS/CDC were to stop enforcing its quarantine and isolation authorities, stop conducting contact investigations among travelers exposed to quarantinable communicable diseases, and if it were unable to implement enhanced entry risk assessment and management programs if warranted by a quarantinable communicable disease outbreak in another country. HHS/CDC cannot quantify the change in risk to the United States that would result, but believes the Korean MERS outbreak is a useful example of the unpredictable course of quarantinable communicable disease outbreaks in the United States.
HHS/CDC estimates that all patients would be hospitalized resulting in treatment costs of around $2.9 million inpatient based on 186 laboratory-confirmed infections and ten days of hospitalization per case. HHS/CDC assumes that the inpatient cost is $1,542 per day based on the costs of treating multidrug resistant tuberculosis in the United States (Table 46). [138]
| Number of people who are infected | Daily inpatient costs | Median duration of hospitalization | Cost of hospitalization |
|---|---|---|---|
| a Korea Centers for Disease Control and Prevention. Middle East Respiratory Syndrome Coronavirus Outbreak in the Republic of Korea, 2015. Osong Public Health Research Perspective. 2015;6(4):269-78. | |||
| b Marks S.M., Flood J., Seaworth, B., et al. Treatment practices, outcomes, and costs of multidrug-resistant and extensively drug-resistant tuberculosis, United States, 2005-2007. Emerging Infectious Disease. 2014; 20(5):812-820. | |||
| (A) a | (B) b | (C) a | (A × B × C) |
| 186 | $1,542 | 10 | $2,868,843 |
The costs associated with excess mortality of the outbreak are estimated at $357.2 million based on the 38 reported MERS-associated deaths reported and a $9.4 million estimate for the value of a value of statistical life. Using a range of $4.3 million to $14.2 million for the value of statistical life, the cost of MERS-associated deaths can be estimated at $163—$540 million (Table 47).
| Best estimate | Lower bound | Upper bound | References | |
|---|---|---|---|---|
| a Korea Centers for Disease Control and Prevention. Middle East Respiratory Syndrome Coronavirus Outbreak in the Republic of Korea, 2015. Osong Public Health Research Perspective. 2015;6(4):269-78. | ||||
| Number of deaths (A) | 38 | 38 | 38 | Korea CDC 2015.a |
| Value of statistical life (B) | $9.4 million | $4.3 million | $14.20 million | Value of statistical life. |
| Mortality cost (A × B) | $357.2 million | $163.4 million | $539.6 million | N/A. |
To arrest the progress of the Korean MERS outbreak as quickly as possible, at least 16,000 people underwent in-house quarantine in South Korea. [139] HHS/CDC assumes that state and local public health departments may implement similar measures if faced with a large outbreak of a newly-introduced quarantinable communicable disease in the United States. The South Korean government recommended 14 days of in-house quarantine based on the incubation period of MERS coronavirus and HHS/CDC assumes that state and local health departments in the United States would implement similar measures. The average wage reported in the Bureau of Labor Statistics, May 2015 Occupational Employment Statistics is $23.23 per hour. [140] Assuming the productivity losses associated with in-home quarantine can be estimated based on the average hourly wage, HHS/CDC estimates the productivity losses at $41.6 million (Table 48).
| Description | N | Reference |
|---|---|---|
| a Korea Centers for Disease Control and Prevention. Middle East Respiratory Syndrome Coronavirus Outbreak in the Republic of Korea, 2015. Osong Public Health Research Perspective. 2015;6(4):269-78. | ||
| b Bureau of Labor Statistics (http://www.bls.gov/oes/current/oes_nat.htm.) | ||
| Number of people who undergo house quarantine (A) | 16,000 | Korea CDC 2015.a |
| Number of days undergo house quarantine per person (B) | 14 | Korea CDC 2015.a |
| Working hours per day (C) | 8 | Assumption. |
| Hourly labor cost (D) | $23.23 | Bureau of Labor Statistics.b |
| Cost of quarantine (A × B × C × D) | $41,628,320 | N/A. |
As of June 10th 2015, a reported 918,000 students, under 19 years of age, were affected by school closure due to the MERS outbreak in South Korea. [141] HHS/CDC cannot predict whether an outbreak with a magnitude similar to the MERS outbreak in South Korea would lead to significant school closures in the United States, but notes that school closures occurred in the United States after the initial Ebola cases in the United States were diagnosed.
During the 2009 H1N1 pandemic in the United States, HHS/CDC initially recommended dismissal of students for at least seven days [142]after the diagnosis of an H1N1 case in a student. Later, HHS/CDC revised the recommendation and school closing was no longer recommended. [143] For the H1N1 outbreak, around 17% of households reported lost work time because of school closure in New York City. [144]In the absence of better data, HHS/CDC assumes schools would be closed for an average of seven days and that each closed school day results in 0.17 missed workdays for a parent. HHS/CDC estimates the productivity loss of parents due to school closure at $203 million (Table 49).
| Description | N | Reference |
|---|---|---|
| a Cho K.Y., Yoo J.S. Forecasting Economic loss associated with MERS outbreak in South Korea, 2015. KERI Insight. 15-20. | ||
| b Borse H.R., Behravesh C.B., Dumanovsky T. et al., Closing schools in response to the 2009 pandemic influenza A H1N1 virus in New York City: Economic impact on households. Clinical Infectious Disease: 2011; 52 (Supple 1) S168-S172. | ||
| c Bureau of Labor Statistics (http://www.bls.gov/oes/current/oes_nat.htm). | ||
| Number of students under 18 years old who were affected by school closure (A) | 918,000 | KERI Insight 2015.a |
| School closure days (B) | 7 | Assumption. |
| Number of loss days of parents per children (C) | 0.17 | Borse et al. 2011.b |
| Working hours per day (D) | 8 | Assumption. |
| Hourly labor cost (E) | $23.23 | Bureau of Labor Statistics.c |
| Cost of quarantine (A × B × C × D × E) | $203,015,033 | N/A. |
In addition to the measurable impacts directly tied to the MERS outbreak. South Korea experience a significant decrease in the number of foreign travelers. The outbreak started in May 2015, but the biggest impacts were observed from June to August when the number of travelers decreased by 26.5% to 53.5% relative to 2014 (Table 50). [145] As the outbreak subsided, the number of travelers returned to previous trends. By September 2015, South Korea only received 10% fewer travelers compared to September 2014. HHS/CDC examined travel data to Dallas in October 2014 (corresponding to the time period in which three Ebola cases were reported), but found no significant difference relative to October 2013. This indicates that the Ebola cases in the United States were not as disruptive as the MERS outbreak cases in South Korea.
| 2014 | 2015 | Change (%) | |
|---|---|---|---|
| June | 1,274 | 751 | −41.0 |
| July | 1,355 | 630 | −53.5 |
| August | 1,454 | 1,069 | −26.5 |
Given all of the above information, South Korean economic modelers attempted to estimate the impact of the MERS outbreak on South Korean GDP in 2015 and estimated that the MERS outbreak alone reduced GDP by 0.26%. [147] If a similar size outbreak occurs in the United States and results in a 0.26% loss to GDP, the economic cost could be extrapolated to be 0.0026 × $17.95 trillion [148] = $41.3 billion.
Summary Ebola Enhanced Entry Risk Assessment and Management Program
The above summary demonstrates the types of analyses that HHS/CDC would undergo when deciding to implement enhanced entry risk assessment and management programs in the future. HHS/CDC will weigh the costs of such programs, the public willingness to accept risks associated with incident cases of quarantinable communicable diseases, the ability of enhanced entry risk assessment and management programs to reduce such risks, and the economic costs of a significant outbreak of a newly-introduced quarantinable communicable disease in the United States. HHS/CDC cannot easily assess how the U.S. public will respond to communicable disease threats and how anxiety associated with communicable disease threats may impact the broader economy.
At the time the Ebola risk assessment program was implemented, HHS/CDC had already been supporting the implementation of exit screening in countries with widespread Ebola transmission for two months. HHS/CDC began support efforts after an ill traveler flew on a commercial flight and introduced Ebola to Nigeria in July 2014. The exit screening efforts in countries with widespread transmission may have resulted in a significant reduction in the number of exported Ebola cases. Only four cases of Ebola (among approximately 300,000 travelers from August 2014) were exported by countries with widespread transmission after the implementation of exit screening and none of these Ebola patients were symptomatic during commercial travel. This can be compared to estimates of 2.8 infected travelers departing Liberia, Sierra Leone, and Guinea each month in the absence of an exit screening program. [149]
The willingness and ability of affected countries to implement effective exit screening will also be considered by HHS/CDC when deciding whether to implement an enhanced entry risk assessment and management program in the future. It will always be a challenge to weigh the costs of public health interventions to the benefits of avoiding a large outbreak of a newly-introduced quarantinable communicable disease. However, HHS/CDC intends to use available evidence such as that summarized above when making decisions.
More Restrictive Alternative: Suspension of Entry during Period West Africa Ebola Outbreak
The more restrictive alternative relative to the NPRM would be for the United States to temporarily suspend the entry of travelers into the United States in the event of widespread transmission of quarantinable communicable diseases. A number of U.S. politicians advocated for this response to the 2014-16 Ebola outbreak in Liberia, Sierra Leone, and Guinea. [150] Some states actively discouraged persons from visiting their states including one example in which prospective participants at a large tropical medicine scientific conference were advised not to travel to a particular state to attend the conference if they had been in one of the countries with widespread transmission within the previous 21 days. [151] The costs and benefits of this alternative are difficult to weigh. Presumably, the costs incurred to implement the Ebola Enhanced entry risk assessment and management program would not have been incurred representing a potential savings (avoided costs) of about $109 million (Table 46). In addition, state and local health departments would not have incurred costs associated with active monitoring of individuals arriving from Ebola-affected countries for a period of 21 days. HHS/CDC does not have any data to estimate these costs, but the costs were probably at least twice the costs for HHS/CDC to implement the Ebola Enhanced entry risk assessment and management program. The costs of state-level active monitoring are estimated as a range from 2 to 4 times the cost of the Ebola enhanced entry risk assessment and management program. The benefits ($327 to $545 million) for the more restrictive alternative are summarized in Table 51.
| Best estimate | Lower bound | Upper bound | ||
|---|---|---|---|---|
| [Suspension of entry] | ||||
| Ebola Enhanced entry risk assessment and management program | $109,003,711 | $109,003,711 | $109,003,711 | |
| Avoided cost of state-level active monitoring | 327,011,133 | 218,007,422 | 436,014,844 | |
| Total benefits | 436,014,844 | 327,011,133 | 545,018,555 | |
Effect on Ebola Risk in the United States
HHS/CDC cannot fully quantify the impact of a travel suspension on the risk of incident Ebola cases in the United States. Modeling studies suggest that travel restrictions would likely have only delayed, but not prevented the spread of Ebola to new countries. [152]
The implementation of travel suspensions would have delayed efforts to stop the outbreak in West Africa by requiring all U.S. volunteers as well as Federal employees to spend 21 days in a designated safe facility or other location outside the United States after working in countries with widespread Ebola transmission. This would surely have dis-incentivized participation in the response. In addition, HHS/CDC cannot predict whether other countries would have followed the U.S. lead in suspending travel. However, HHS/CDC believes that travel suspensions would have delayed outbreak response efforts and may have been more likely to lead to additional spread of Ebola especially to neighboring countries in Africa.
Under this alternative, traveler opportunity costs would be much greater because any travelers to countries with widespread Ebola transmission would no longer be allowed to enter the United States for a period of 21 days. If there is no decline in travelers, each traveler loses approximately 21 days of productivity as a result of the suspension, traveler opportunity costs can be estimated by 38,334 travelers × 8 hours per day × 21 days × $23.23 (average U.S. wage rate) = $150 million. These costs alone could more than offset the cost of Ebola Enhanced entry risk assessment and management program. The cost for those travelers to spend an additional 21 days at a secure location would probably be similar to the opportunity cost estimate from above or more depending of operating a designated safe facility or the cost of staying at another location outside the United States.
However, this simplistic analysis probably does not accurately reflect the implications of a travel suspension. Suspension of entry would probably significantly reduce the number of U.S. volunteers willing to travel to West Africa to mitigate the Ebola outbreak closer to its sources. This would delay the progress made in suppressing the outbreak and increase risk of exportation to other countries. HHS/CDC cannot predict how other countries may have responded to the U.S. decision to suspend entry. If other countries implemented similar restrictions, there may have been a chain of reaction leading to a significant decrease in the number of global volunteers to the most affected countries. In this scenario, the 2014-16 Ebola outbreak in West Africa would have almost certainly persisted for a much longer period of time. HHS/CDC cannot estimate the long term impact for the affected countries, the West African region, or the costs to the U.S. government or its people.
While HHS/CDC is not able to estimate a dollar value of diminished trade in general, the estimated trade volumes prior to the outbreak are available and summarized in Table 52. The total annual value of trade for the three Ebola-affected countries in West Africa is $574 million and ranges from $125 million with Sierra Leone to $270 million with Liberia. [153]
| Country | Trading partner rank | Value U.S. exports to country | Description of U.S. exports | Value of U.S. imports to country | Description of U.S. Imports | Total value imports + exports |
|---|---|---|---|---|---|---|
| a Data extracted from the U.S. Office of the Trade Representative 154 | ||||||
| Guinea | 153 | $80M | Vehicles, machinery | $99M | Metals and precious stones | $179M |
| Liberia | 142 | 173M | Machinery, iron/steel, vehicles | 97M | Rubber, salt/sulfur, precious stones | 270M |
| Sierra Leone | 162 | 83M | Machinery, vehicles, meat | 42M | Ores, metals, precious stones | 125M |
It is likely that U.S. economic losses would be much less than the numbers reported in Table 53 because U.S.-based importers and exporters would still be able to import or export some goods or services while the temporary travel delay remains in place. There may also be some substitution of countries by U.S. firms, for example if a particular good is made or grown in more than one country, U.S. firms might shift their purchasing away from one trade partner to the other. However, once purchasing is shifted there may be future difficulties once the suspension of entry is lifted if there are negative political consequences.
In the absence of data HHS/CDC assumes that the cost of lost trade for a one-year period can be estimated by a range of 0.1%, 1%, or 10% of lost trade (minimal to maximum, Table 53). Generally, the losses in the three countries with widespread Ebola transmission are estimated to range from about $0.55 million to $55 million.
| Country | Total value imports + exports | Assumed financial losses to U.S. stakeholders as % of total trade | ||
|---|---|---|---|---|
| 10% | 1% | 0.10% | ||
| Guinea | $179M | $17.9M | $1.79M | $0.179M |
| Liberia | 270M | 27.0M | 2.70M | 0.270M |
| Sierra Leone | 125M | 12.5M | 1.25M | 0.125M |
| Subtotal | 574M | 57.4M | 5.74M | 0.547M |
| Best estimate | Lower bound | Upper bound | |
|---|---|---|---|
| a This lower bound assumes that half of the travelers decided not to go to West Africa. | |||
| b The estimated lodging costs are assumed to be similar in magnitude to the opportunity costs. | |||
| Opportunity costs to travelers | $149,643,000 | a $74,821,500 | $149,643,000 |
| Lodging costs for 21 days outside the United States or at a designated safe facility b | 149,643,000 | 74,821,500 | 149,643,000 |
| Trade costs | 5,470,000 | 547,000 | 55,470,000 |
| Total quantified costs | 304,756,000 | 150,190,000 | 354,756,000 |
Comparing the costs in Table 51 and benefits in Table 54, the most easily quantified benefits may be greater than the most easily quantified costs. However, given the potential other costs associated with prolonging the length of the Ebola outbreak in West Africa, the potential for other countries to implement travel restrictions after the United States, and the potential that delayed cessation of the Ebola outbreak could have led to serious political and economic outcomes in West Africa, HHS/CDC believes that the suspension of entry would have been a poor alternative to the implementation of the Ebola Enhanced entry risk assessment and management program to reduce the risk of Ebola transmission in the United States. Suspension of entry could enhance the United States future vulnerability to communicable disease threats if other countries would have observed this suspension of entry and tried to conceal communicable disease outbreaks within their borders. This potentially reduced ability to address future communicable disease threats in combination with the realization that only two Ebola cases associated with international commercial travel occurred in the United States under the status quo, HHS/CDC believes that implementation of travel suspensions will lead to more costs than benefits relative to the status quo. However, HHS/CDC cannot quantify all of the costs and benefits of travel suspensions. HHS/CDC solicits public comment about the costs and benefits of a suspending entry as an alternative to HHS/CDC’s decision to implement the Ebola Entry Risk Assessment program.
Payment for Care and Treatment (Proposed 42 CFR 70.13/71.30)
The revisions to 42 CFR 70.13/71.30: Payment for Care and Treatment are not expected to lead to a change in HHS/CDC policy under which HHS/CDC may act as the payer of last resort for individuals subject to medical examination, quarantine, isolation, and conditional release under Federal orders. The primary benefit of codification is increased transparency around HHS/CDC policies to assist in paying for treatment for individuals under Federal orders.
The provisions included in the NPRM are similar to a Memorandum of Agreement between a number of hospitals and HHS/CDC. Under the terms of the Memorandum of Agreement, the hospital can be reimbursed for incurred medical expenses subject to HHS/CDC’s discretion, availability of appropriations, and limited to what a hospital would bill Medicare. The Memorandum of Agreement also indicates that HHS/CDC should be the payer of last resort.
HHS/CDC issued 12 isolation orders between Jan. 1, 2005 and May 10, 2016, which would correspond to an average of about 1 order per year over the past 11.3 years. HHS/CDC has information on payments made for 3 of the 12 cases. In most cases, HHS/CDC makes payment directly to healthcare facilities, sometimes in lieu of payments that would be made by state or local health departments. Among the three instances for which HHS/CDC has some data on payments for treatment, care, and transportation of individuals under Federal orders:
- In one case, HHS/CDC paid $7,000 for a patient’s care after splitting the cost with a local health department.
- In a second case, HHS/CDC paid over $200,000 of the treatment costs.
- In a third case, HHS/CDC paid healthcare facilities directly for treatment and transport of an individual who had been paroled into the United States. In this situation, HHS/CDC paid approximately $80,000 for this patient’s transport and treatment.
HHS/CDC could not confirm whether it paid for treatment for any of the 9 other individuals under Federal orders in the previous 11.3 years. It is possible that HHS/CDC did help pay for treatment for some of these individuals. HHS/CDC’s expected annual payments for care and treatment are estimated to be between 0 and $1,000,000 in any given year under the current baseline. This upper bound cost would correspond to a year in which HHS/CDC would have to incur the costs of two patients at $500,000 per patient. This roughly corresponds to the average cost to treat an extremely drug-resistant tuberculosis case (XDR-TB). [155] Alternatively, this could represent a situation in which HHS/CDC may have to pay a significant fraction of the total costs for one very complicated illness associated with a quarantinable communicable disease not endemic to the United States (e.g., Ebola).
To estimate the average annual payments for care and treatment by HHS/CDC, the average payment for the three cases with known payment information can be assumed to be incurred annually (corresponding to the average number of isolation orders that HHS/CDC issues each year). In this case, the average annual cost to the Federal government would be ($7,000 + $80,000 + $200,000)/3 years = ~$96,000 per year. If instead HHS/CDC assumes zero payments by CDC for the other nine cases for which it is unclear whether or not CDC paid any amount, the average annual cost would be ($7,000 + $80,000 + $200,000)/12 years = ~$24,000 per year. HHS/CDC can estimate with some certainty that the current annual average costs to the Federal government are probably somewhere in the range of $24,000 to $100,000 and not likely to exceed $1,000,000 in any one year.
HHS/CDC has not incurred any costs for the care and treatment of any individuals besides for those under Federal isolation orders.
When HHS/CDC assumes responsibility to pay for treatment as the payer of last resort, another entity, typically a healthcare facility or state/local health department, would incur a benefit exactly equal to the amount of the HHS/CDC payment. This is referred to as a transfer payment, because from the perspective of the U.S. economy, there is zero net cost or benefit, simply a transfer from the Federal government to another entity.
The codification of 42 CFR 70.13 and 42 CFR 71.30 is not expected to change HHS/CDC’s policy to continue to act as the payer of last resort. However, it may be possible that in the absence of codification, a precedent-setting event may occur in which HHS/CDC must take on additional responsibility to pay for the care and treatment of individuals under Federal orders. HHS/CDC’s best estimate (and lower bound) of the impact of the changes to 42 CFR 70.13 and 42 CFR 71.30 is zero net cost or benefit to HHS/CDC or to healthcare facilities. The upper bound estimate corresponds to a 50% increase in HHS/CDC’s average cost estimate for payments for care and treatment (50% × $96,000 = $48,000). In this case, without the NPRM, HHS/CDC could incur additional costs of up to $48,000 per year. If HHS/CDC is incurring additional costs, healthcare facilities would receive a corresponding benefit in receiving payments from HHS/CDC. Thus, without the NPRM, healthcare facilities may receive up to an average $48,000 in additional payments from HHS/CDC for the care and treatment of individuals under Federal orders. Thus, with the NPRM, an upper bound estimate of benefits to HHS/CDC would be $48,000 from the implementation of the NPRM. The corresponding upper bound estimate of costs to healthcare facilities associated with implementation of the NPRM would be $48,000. An extreme upper bound economic impact of the NPRM for any one year would be a benefit to HHS/CDC of avoided payments equal to $500,000 and a corresponding cost to healthcare facilities of $500,000 representing losses associated with treatment costs incurred for one additional XDR-TB case [156] (Table 55). XDR-TB is very expensive to treat, because it can take up to two years to resolve. This amount would be similar to the cost to treat one Ebola case. The cost to treat an Ebola patient has been reported to be about $650,000 [157] at the Nebraska Medical Center and has been estimated to exceed $1 million [158] if the cost of Ebola waste disposal is not included. However, because of the severity of Ebola, it is unlikely than an Ebola patient would have to be placed under a Federal order to seek treatment. MERS or SARS are examples of other diseases for which it is possible that patients may be placed under Federal orders; however, the costs of treating these diseases are expected to be considerably less than for XDR-TB or Ebola.
HHS/CDC specifically solicits public comment on cost estimates associated with changes to 42 CFR 70.13/71.30: Payment for care and treatment.
| Marginal benefit to HHS/CDC resulting from NPRM | Marginal cost to U.S. individuals or healthcare facilities resulting from NPRM | Net cost/benefit | ||
|---|---|---|---|---|
| NPRM | Best estimate | $0 | $0 | $0 |
| Lower bound | 0 | 0 | 0 | |
| Upper bound | 48,000 | 48,000 | 0 | |
| Extreme upper bound | 500,000 | 500,000 | 0 | |
| Less Restrictive Alternative (Cost estimate to pay for all Travelers sent to hospitals for evaluation during a potential enhanced entry risk assessment and management program) | Best estimate Lower bound Upper bound | (1,885,000) (471,250) (9,425,000) | 1,885,000 471,250 9,425,000 | 0 0 0 |
| More Restrictive Alternative (HHS/CDC never pays for care or treatment for persons under Federal orders) | Best estimate Lower bound Upper bound | 48,000 24,000 96,000 | 48,000 24,000 96,000 | 0 0 0 |
HHS/CDC examines two alternatives to codification of its current policy that individuals under Federal orders will utilize third party resources first. Under the first, less restrictive alternative, HHS/CDC would pay for individuals to be tested at hospitals if referred from an enhanced entry risk assessment and management program at airports in the future (i.e., similar to the 2014-16 Ebola enhanced risk assessment program). Under the more restrictive alternative HHS/CDC would never offer to pay for treatment and care.
Besides the NPRM analysis included in Table 55, the Federal burden to pay for care and treatment may have included persons sent to hospitals from airports for further evaluation during the Federal government’s Ebola enhanced entry risk assessment and management program. Over the 16 month period of this program, a total of 29 travelers out of 38,344 screened (0.08%) were recommended for transport from the airport to a hospital for further testing. All travelers complied voluntarily and Federal orders were not issued. HHS/CDC does not have any data to estimate the cost of transportation to and evaluation at hospitals. The cost to treat Ebola patients was reported to be about $30,000 per day at the Nebraska Medical Center and about $50,000 per day at the National Institutes of Health. [159] If the daily cost of evaluation is estimated to be similar to the cost of treating Ebola patients (i.e., $30,000-$50,000 per day) and it is assumed that evaluation requires 24-48 hours, a lower bound cost estimate for evaluation would be $30,000/day × 1 day = $30,000 and an upper bound cost estimate could be calculated from $50,000/day × 2 days = $100,000. The midpoint cost estimate is $65,000. For 29 patients at the midpoint cost estimate, the total cost is 29 patients × $65,000 per patient = $1,885,000.
For the less restrictive alternative, HHS/CDC assumes a best estimate that is the same as the expected cost for hospital follow-up as part of the 2014-16 Ebola enhanced risk assessment program. This is not an annual cost since HHS/CDC does not perceive that it is likely to implement enhanced risk assessment programs on an annual basis in the future. For the lower bound estimated cost in a one-year period if an enhanced risk assessment program is implemented, HHS/CDC assumes a cost equal to 25% of that estimated for the Ebola enhanced risk assessment program or $471,250. For an upper bound estimate in any one year, HHS/CDC assumes that the program costs five times more than that estimate for the Ebola risk assessment program or $9,425,000.
If HHS/CDC has to pay these costs, given its fixed budget, other HHS/CDC programs would have to receive less funding. One example of a program that HHS/CDC supports is an overseas vaccination program for refugees. This program was recently introduced by the Division of Global Migration and Quarantine with assistance from interagency partners. Since vaccination is often compulsory for children to attend public schools, most refugee children would have to be vaccinated after arrival in the United States even if HHS/CDC is unable to support overseas vaccination. According to unpublished data, the cost to provide vaccines in countries from which refugees travel to the United States is much lower than the U.S. vaccination costs even using Medicaid reimbursement rates. The 2015 price of measles mumps and rubella vaccine available from UNICEF, who supplies most countries from which U.S.-bound refugees travel, is $1.08—$3.25. [160] In comparison, the same vaccine costs $19.90 when publicly procured in the United States. [161] HHS/CDC estimates that the cost of vaccine procurement and delivery for refugees is at least half as expensive overseas compared to domestic vaccination after arrival. In addition, U.S.-bound refugees tend to be at much greater risk of communicable diseases than other international travelers. One study found that the costs associated with a single case imported by a refugee was $25,000. [162]
At the same time, U.S. healthcare payers or state/local health departments would not have to incur the marginal costs that would be paid by HHS/CDC. This could lead to reduced out-of-pocket payments by those that need to be tested or treated and reduced payments for their health insurers. In some situations, costs may be covered as charitable care by treatment facilities if patients are unable to pay.
For the more restrictive alternative, HHS/CDC considers a scenario in which it would never have to pay for care and treatment. This would reduce HHS/CDC’s current estimated payment of $48,000 per year to zero and healthcare treatment facilities or health departments would like have to pay an equivalent amount. The lower bound is half of the estimate of current payments ($24,000) and upper bound is double the average annual payments ($96,000). The societal cost of this alternative is difficult to measure and would depend on whether treatment facilities would begin to refuse to admit patients subject to Federal orders, but not in dire need of treatment (e.g., an undocumented immigrant with infectious tuberculosis with non-life-threatening symptoms).
§ 71.63 Suspension of entry of animals, articles, or things from designated foreign countries and places into the United States
In this NPRM, HHS/CDC is elucidating its authority to temporarily suspend entry of animals, articles or things from designated foreign countries and places into the United States. HHS/CDC cannot predict how often such authority may be used in the future or for what purpose. HHS/CDC exercised this authority on June 11, 2003, “when under 42 CFR 71.32(b), HHS/CDC implemented an immediate embargo on the importation of all rodents from Africa (order Rodentia).” [163]Simultaneously, but unrelated to provisions included in this NPRM, “the Director of CDC and the Commissioner of Food and Drugs, under42 CFR 70.2 and 21 CFR 1240.30 respectively, issued a joint order prohibiting, until further notice, the transportation or offering for transportation in interstate commerce, or the sale, offering for sale, or offering for any other type of commercial or public distribution, including release into the environment, of:
- Prairie dogs (Cynomys sp.);
- Tree squirrels (Heliosciurus sp.);
- Rope squirrels (Funisciurus sp.);
- Dormice (Graphiurus sp.);
- Gambian giant pouched rats (Cricetomys sp.);
- Brush-tailed porcupines (Atherurus sp.); and
- Striped mice (Hybomys sp.).” [164]
Both provisions were necessary to prevent transmission of monkeypox, a rare, zoonotic, viral disease that occurs primarily in the rain forest countries in Central and West Africa. (A zoonotic disease is a disease of animals that can be transmitted to humans under natural conditions.) The illness was first noted in monkeys in 1958, but, in Africa, serologic evidence of monkeypox infection has been found in many other species, including some species of primates, rodents, and lagomorphs (which includes such animals as rabbits). African rodents are considered to be the most likely natural host of the monkeypox virus.[165]
The temporary ban was later codified as a permanent restriction on importation of African rodents and other animals that may carry the monkeypox virus with an exception, which allows importation for scientific, exhibition, or educational purposes if a written request for such importation is approved CDC (existing 42 CFR 71.56). This suspension of import was codified in an interim final rule published on November 4, 2003. [166]
Since the African rodent embargo in 2003, HHS/CDC has implemented only one other embargo. On January 13, 2004, the Department of Health and Human Services (HHS) announced an immediate embargo on the importation of civets to the United States. At the time, civets had been identified as a possible link to SARS transmission in China. [167]
HHS/CDC does not have any data on the number of illegal imports of African rodents or civets during the time the temporary embargos have been in place and no way to quantify the impact of codification of this authority. The African rodent embargo predated the implementation of HHS/CDC’s Quarantine Activity Reporting System, which is used to document its activities. For civets, HHS/CDC has data on four attempted importations for the period from October 13, 2005 through June 10, 2016. Among the four attempted importations, three were allowed to enter the United States with a special permit for science, education or exhibition. The fourth shipment was for commercial purposes. This shipment was denied entry and the animals were returned to the source country. The importer was aware of the civet embargo, but did not realize the animal in question were part of the same family (Viverridae) that are prohibited. HHS/CDC would like to solicit public comment on how behaviors might change with proposed codification under 71.63 with this NPRM compared to HHS/CDC’s reliance on existing 71.32b when implementing temporary animal importation embargos.
The temporary embargo on African rodents implemented on June 11, 2003 provides an example of how HHS/CDC has used existing regulatory authority under 42 CFR 71.32(b), which states that “Whenever the (CDC) Director has reason to believe that any arriving carrier or article or thing on board the carrier is or may be infected or contaminated with a communicable disease, he/she may require detention, disinfection, disinfestation, fumigation, or other related measures respecting the carrier or article or thing as he/she considers necessary to prevent the introduction, transmission, or spread of communicable diseases.” The proposed language under 71.63 would codify how this authority may be applied in the future. Since this provision does not impose any new regulatory burden, the mostly likely economic impact is no change from the current baseline. A qualitative benefit of the proposed 71.63 is improved understanding of how and why HHS/CDC may suspend entry of animals, articles, or things in the future. An estimate of the economic impact of the temporary embargo of African rodents provides an example of the potential economic impact of future restrictions that HHS/CDC may deem necessary to protect public health.
Costs of the African Rodent Embargo
The costs associated with a suspension of imports can be estimated based on the lost value to consumers and producers associated with not being able to import, sell, barter, or exchange African rodents. At the time of prohibition, African rodents were imported primarily for commercial, or science, education and exhibition purposes. In 2002, a total of 11,587 live rodents were imported, and 1,378 of them (around 12%) were from Africa. [168] In 2013, the total number of imported live rodents were 173,761. During this period, there was a shift from wild-caught species, including those of African origin, to other rodent species shipped from multiple countries outside of the African continent. [169] The percentage of wild-captured imports declined from 75% during 1999 to less than 1% during 2013. [170] Although the total market for imported rodents increased by approximately 15 times (1500%), HHS/CDC believes that the market for African rodents would probably not have expanded at the same rate. One reason is that market for African rodents would likely be more of a niche market for exotic pets compared to the overall market for domestic rodents. As a point of comparison, imports from Asian countries experienced a smooth decline during 1999-2013. [171] A second reason is that consumer demand for African rodents would likely decline after the association of African rodents with the risk of contracting monkeypox virus was clearly demonstrated in the U.S. market.
To provide a conservative estimate of the economic cost of the prohibition on imports of African imports, HHS/CDC uses the average number of African rodent imports in the three years prior to the import suspension to estimate the number of imports as the baseline if the import embargo had not been implemented. On average, 959 African rodents per year were imported between 2000 and 2002.
HHS/CDC assumes that the annual cost of the African rodent import embargo can be subdivided into the following three categories: (1) African rodents imported using a special permit from CDC, (2) African rodents that are replaced by other regions’ imported substitutes, and (3) African rodents that cannot be imported with special permits or substituted. The summary of the costs for each category are included in Table 56 and summarized subsequently.
| Source of cost | Costs |
|---|---|
| Importing African rodents using a special permit from CDC | $744 |
| Use of substitute rodents from other regions | 11,900 |
| Lost consumer surplus due to African rodents unavailability | 6,390 |
| Total | 19,034 |
Incremental Costs of Importing African Rodents Using a Special Permit From CDC for Scientific, Educational, or Exhibition Purposes
African rodents that otherwise would be prohibited are eligible for a special permit from the CDC director if they are imported for scientific, educational, or exhibition purposes. Approximately 65 African rodents per year were imported from 2004 to 2013. [172] The HHS/CDC assumes that all these imported African rodents after the ban are used for scientific, educational, or exhibition purposes.
HHS/CDC estimates that the permitting process imposes additional costs that would not be incurred in the absence of the embargo. On an annual basis, the annual cost to obtain a special permit from CDC will result in about $372 in incremental costs based on an assumption that the average hourly wage importer’s hourly wage is $31 and African rodents arrive in three separate shipments. Thus, HHS/CDC assumes that around 20 African rodents are included in each shipment (Table 57). The analysis does not include costs to appeal a permit denial.
| Importer time per shipment (hours) a | Importer’s hourly labor cost | Shipments imported with special permit | Number of African rodents per shipment | Overhead multiplier | Importer cost to request special permit |
|---|---|---|---|---|---|
| a The analysis assumes a greater time burden to request a special permit to import animals that are prohibited because more information is required as a part of this request, including detailed descriptions of travel conditions and other measures taken to prevent the spread of disease. | |||||
| (A) | (B) | (C) | (D) | (E) | (A × B × C × E) |
| 4 | $31 | 3 | 20 | 100% | $744 |
Incremental Costs Associated With the Use of Substitute Rodents
Commercially imported African rodents are expected to be replaced either by imported rodents from other regions or by increased U.S. production of rodents. Most African rodents are exotic species, and are not commonly imported rodents relative to the more commonly imported hamsters, guinea pigs, or cavies. [173] HHS/CDC assumes that all substitutes would be imported from countries other than Africa and would not be replaced by domestically produced substitutes.
The estimated price of imported non-African rodents is $20. According to 2012 data contained in the U.S. Fish and Wildlife Service’s (USFWS) Law Enforcement Management Information System (LEMIS), 75 percent of rodents imported in 2008 were hamsters, and another 3 percent were chinchillas. A sample of prices for rodents advertised online yielded an average cost of about $15 for hamsters and an average cost of $142 for chinchillas. The weighted average price of these animals is around $20. Since African rodents are exotic species, HHS/CDC assumes that the price of African rodents is higher than the average price of imported non-African rodents. Thus, HHS/CDC uses the average price of chinchillas, which is about seven times greater than the estimated price of more commonly purchased rodents. In addition to the potential price increase associated with imports from other regions, U.S. consumers may also derive less utility from substitutes for African rodents. HHS/CDC estimates substitution costs by assuming that these costs are 10% of the estimated price of African rodents (based on chinchillas). As a result, U.S. consumers would have to pay approximately $14 more or lose $14 in utility for each substituted rodent import in place of the African rodents that would be purchased in the absence of an embargo (Table 58).
| Incremental cost per African rodent a | Number of rodents bsubstituted | Total incremental cost |
|---|---|---|
| a $142 × 10%. | ||
| b 894 of commercially imported African rodents × 95%. | ||
| (A) | (B) | (A × B) |
| $14 | 850 | $11,900 |
Incremental Costs of Lost use due to African Rodents’ Unavailability
HHS/CDC assumes that substitutes are not available for 5% of commercially imported African rodents. The absence of these animals will result in lost profit for the affected importers and lost utility to the affected consumers. HHS/CDC assumes that the average price can be used to estimate these costs, although HHS/CDC acknowledges that this may be an underestimate because lost consumer surplus is likely to be greater than the average price. HHS/CDC estimates the cost of lost consumer surplus associated with the lack of acceptable substitutes for U.S. consumers who can no longer import African rodents at 45 × $142 = $6,390 (Table 59).
| Incremental cost per unavailable African rodent a | Number of African rodents becoming unavailable b | Total incremental cost |
|---|---|---|
| a HHS/CDC adapted price of chinchillas for the price of unavailable African rodents | ||
| b 894 commercially imported African rodents × 5% | ||
| (A) | (B) | (A × B) |
| $142 | 45 | $6, 390 |
Benefits of the African Rodent Embargo
The economic benefits of the African rodent embargo are likely much greater than the estimated costs. The primary benefits are improvements to human and animal health in the United States, averted public health measures necessary to contain a monkeypox outbreak, and averted costs to other animal markets in case of transmission of monkeypox from African rodents to other species through intermingling in the pet industry. The 2003 monkeypox outbreak resulted in a total of 71 cases that were clinically or laboratory confirmed. [174] Among the 71 total cases, 16 patients (23%) with monkeypox infections were admitted to hospitals for treatment or for isolation. Two patients had serious clinical illness, but subsequently recovered and no deaths associated with monkeypox were reported.[175] The two severe cases occurred in children who required intensive care, one for severe monkeypox-associated encephalitis (encephalitis is an inflammation of the brain), and one with profound painful cervical (neck) and tonsillar adenopathy (adenopathy refers to an enlargement of the glands) and diffuse pox lesions, including lesions in the throat.[176] Otherwise, the clinical symptoms of monkeypox included skin lesions with fever (temperature above 38 °C, 100.4 °F), drenching sweats and severe chills, headache, sore throat and persistent coughing. Other less common symptoms included lymphadenopathy (swollen glands), mild chest tightness, tonsillar erosion, general body malaise, myalgia (muscle aches), back pain and nasal congestion. [177]
The number of monkeypox cases was increasing over an approximately 3-week period from the identification of the first case on May 15, 2003 through the week ending June 8, 2003. The number of cases declined subsequently; the date of onset for the last case was June 20, 2003. [178] In the United States, individuals apparently began contracting monkeypox, primarily as a result of contact with prairie dogs that had contracted monkeypox from diseased African rodents. Investigations indicate that a Texas animal distributor imported a shipment of approximately 800 small mammals from Ghana on April 9, 2003, and that shipment contained 762 African rodents, including rope squirrels (Funiscuirus sp.), tree squirrels (Heliosciurus sp.), Gambian giant pouched rats (Cricetomys sp.), brushtail porcupines (Atherurus sp.), dormice (Graphiurus sp.), and striped mice (Hybomys sp.). Some animals were infected with monkeypox, and CDC laboratory testing confirmed the presence of monkeypox in several rodent species, including one Gambian giant pouched rat, three dormice, and two rope squirrels. Of the 762 rodents from the original shipment, 584 were traced to distributors in six states. A total of 178 African rodents could not be traced beyond the point of entry in Texas because records were not available. [179]
Non-native animal species, such as African rodents, can create serious public health problems when they introduce a new disease, such as monkeypox, to the native animal and human populations. The transportation, sale, or distribution of an infected animal, or the release of an infected animal into the environment can result in the further spread of disease to other animal species and to humans. Several States issued orders or emergency rules to prohibit the importation, sale, distribution, release, disposal, and/or display of prairie dogs and certain rodents. 180 181 182 183 184 185
The monkeypox outbreak was contained in the United States after CDC and the public health departments in the affected states, together with the U.S. Department of Agriculture, the Food and Drug Administration, and other agencies, participated in a variety of activities that prevented further spread of monkeypox.
To assist with the investigation and outbreak response, CDC took the following steps in addition to the embargo on the importation of African rodents:
- Activated its Emergency Operations Center.
- Deployed teams of medical officers, epidemiologists, and other experts to several states to assist with the investigation.
- Conducted extensive laboratory testing on specimens from humans and animals thought to have been exposed to monkeypox.
- Issued interim U.S. case definitions for human monkeypox and for animal monkeypox.
- Issued interim guidelines on infection control and exposure management for patients in the health care and community settings.
- Issued an immediate embargo and prohibition on the importation, interstate transportation, sale, and release into the environment of certain rodents and prairie dogs.
- Provided ongoing assistance to state and local health departments in investigating possible cases of monkeypox in both humans and animals the United States.
- Worked with state and Federal agencies to trace the origin and distribution of potentially infected animals.
- Issued an interim guidance on the use of smallpox vaccine (which also can be used to protect people against monkeypox), cidofovir (an antiviral medication), and vaccinia immune globulin (an antibody product obtained from the blood of people who have received the smallpox vaccine) in the setting of an outbreak of monkeypox.
- Issued interim guidelines for veterinarians.
- Issued interim guidance for persons who have frequent contact with animals, including pet owners, pet shop employees, animal handlers, and animal control officers. [186]
These activities suggest the scale of the response required to contain monkeypox and the potential threat posed by the importation of African rodents. The public health response is estimated to require at least 20 HHS/CDC employees over a 2.5 month period. These employees are assumed to be compensated at the GS-13, step 5 level on average. In addition, the total number of personnel from public health departments in the six affected states are assumed to at least equal the number of HHS/CDC employees. The average wage rate for public health departments is estimated based on 2015 U.S. average wage rates for epidemiologists reported in the May 2015 National Occupational Employment and Wage Estimates from the Bureau of Labor Statistics ($36.97, category 19-1041). [187] Total costs for the public health response include a 100% multiplier to account for overhead costs for these employees, but do not include potential travel and per diem costs that may have been incurred to investigate the outbreak. The total costs to HHS/CDC and public health departments are summarized in Table 60.
| Number of employees | Duration (months) | Average hourly wage rate | Overhead multiplier (%) | Total cost | |
|---|---|---|---|---|---|
| HHS/CDC employees | 20 | 2.5 | $47.36 | 100 | $757,760 |
| State or local health departments | 20 | 2.5 | 36.97 | 100 | 591,520 |
| Total | $1,349,280 |
The list of HHS/CDC activities referenced above include guidance provided to veterinarians, persons who have frequent contact with animals including pet owners, pet shop employees, animal handlers, and animal control officers. It is likely that all of these stakeholders incurred costs as a result of the monkeypox outbreak; however, HHS/CDC does not have data to quantify most of these costs. HHS/CDC does have some data for one set of affected stakeholders. The size of the prairie dog market was estimated to be approximately $4.5 million in 2003, [188] which would correspond to $5.8 million in 2015 USD after adjustment using the U.S. Consumer Price Index. Considering only the disruption to the prairie dog market, HHS/CDC estimates that the cost to this market would be at least 25% of the total market size in any year in which monkeypox transmission was associated with sales of prairie dogs. This large cost is estimated because infection of prairie dogs led to significant restrictions on interstate transport of prairie dogs and because several states issued orders or emergency rules to prohibit the importation, sale, distribution, release, disposal, and/or display of prairie dogs. This one-time 25% reduction would correspond to an annual cost of about $1.5 million just to this one market in the event of a re-introduction of monkeypox to the United States and transmission within the prairie dog population.
The treatment costs for individuals diagnosed with monkeypox or exposed to infected persons or animals include hospitalization, outpatient treatment, medications, vaccinations (with smallpox vaccine), laboratory diagnosis, and the opportunity costs to individuals who contract monkeypox and cannot undertake their normal daily activities. Laboratory diagnosis of monkeypox can involve multiple approaches including combined Polymerize Chain Reaction (PCR) tests, enzymes-linked immunosorbent assays (ELISA) tests, DNA extraction of tissues to perform molecular tests and others. Most of the patients with monkeypox disease were treated with antibiotics (ciprofloxacin and doxycycline) and a few patients received intravenous acyclovir and valacyclovir medications. [189] The costs of treating monkeypox were not systematically documented. [190]
Table 61 provides a rough estimate of potential illness costs associated with an outbreak of monkeypox of similar size to the outbreak that occurred in 2003. The documented costs include 56 cases treated on an outpatient basis in emergency rooms at an estimated cost of $1,455 per patient. [191] This estimate is based on the U.S. average cost for an outpatient hospital visit for any illness and is probably a very conservative estimate of the outpatient cost of treating monkeypox. Hospitalization costs are estimated at $16,516 per patient for each of 16 cases based on the average cost of hospitalization for any illness. [192]Again, this cost estimate is probably very conservative for monkeypox treatment.
All individuals (outpatients and inpatients) who contract the disease are estimated to lose an average of 12 days of productive activity. This assumption is based on a clinical report that on average infected individuals were ill for between 3 to 24 days. [193] To be conservative, HHS/CDC only includes lost productivity costs for adults. Among laboratory confirmed monkeypox cases, 11 out of 35 (31%) patients occurred in patients less than 18 years old. Applying this ratio to the total number of cases (71), approximately 49 adults would incur lost productivity costs. For each adult, average productivity costs are estimated based on the U.S. average hourly salary ($23.23) reported in the 2015 Occupational Employment Statistics from the U.S. Bureau of Labor Statistics [194] and assuming an 8-hour workday. Productivity losses are then estimated based on the average wage rate × 12 days × 8 hours per day × number of monkeypox patients ($108,531). The total illness are estimated to be about $453,000 (Table 61).
| Activity | Units | Unit cost a | Total costs |
|---|---|---|---|
| a Unit costs updated to USD 2015 using the U.S. Consumer Price Index where appropriate. | |||
| (A) | (B) | A × B = (C) | |
| Outpatient treatment, ER Visit Cost 195 | 196 55 | $1,455 per patient | $80,025 |
| Hospital stay 197 | 198 16 | 16,516 per patient | 264,256 |
| Lost productivity | 48.7 (69%) for 584 Days | 161.68 per patient-day | 108,531 |
| Total costs | 452,812 | ||
The total quantified costs associated with the 2003 monkeypox outbreak are summarized in Table 62. These include a partial accounting of the costs incurred to HHS/CDC and to local public health departments, a one-time estimate of the potential costs to the U.S. prairie dog market, and a conservative estimate of illness costs for persons infected with monkeypox ($3.3 million).
| Public health response costs | $1,349,280 |
| One-time costs to prairie dog market in the United States | 1,500,000 |
| Illness costs | 452,812 |
| Total | 3,302,092 |
The outbreak costs reported in Table 62 represent a very conservative estimate of the potential benefits of reducing the probability of a future re-introduction of the monkeypox virus into the United States. The total costs of such an outbreak would probably greatly exceed the conservative estimates presented in Table 62. Since the order to embargo the importation of African rodents in June 2003 and subsequent permanent restriction on the importation of African rodents codified in existing 42 CFR 71.56, the monkeypox virus has not been reintroduced to the United States. Comparing the potential benefits of an averted monkeypox outbreak in Table 62 ($3.3 million) to the estimated costs to African rodent importers and potential consumers (Table 56, $19,000), it is extremely likely the benefits of the African rodent import prohibition would greatly exceed the costs. However, HHS/CDC is not able to quantify the risk of re-introduction with and without the restrictions on African rodent imports. Although this NPRM only seeks to codify HHS/CDC’s ability to suspend entry of animals, articles, or things from designated foreign countries and places into the United States based on existing 42 CFR 71.32(b), this example demonstrates the potential costs and benefits of one such action. Because this outbreak occurred about 13 years ago, HHS/CDC specifically solicits public comment on cost estimates associated with the prohibition of African rodent imports and the cost of the 2003 monkeypox outbreak.
Evaluation of Alternatives
Two potential alternatives are considered to codification of this provision in the NPRM. Under the first less restrictive alternative, HHS/CDC would not implement temporary embargos after it becomes aware of imminent risks to public health in the United States. Under this scenario, there would be no embargo on the importation of African rodents between June 11, 2003 and November 4, 2003. Under this scenario, the United States would have remained at risk for the re-introduction of monkeypox virus and the need to eliminate the virus from the United States animal and human populations. This scenario is elaborated above.
The more restrictive alternative would be for HHS/CDC to no longer consider special permits to allow importation for scientific, education, and display purposes. HHS/CDC believes that limiting importations to these purposes protects public health, while allowing importation to occur in very controlled environments. If special permits were discontinued, African rodent importers would no longer have to fill out import permits at an annual cost of $744 (Table 57). This is the cost to create three special permit applications per year.
In comparison, civet shipments with special permits occur approximately once every three years, so the annual cost to create special permits is $744/9 = $83 for civets. However, importers would no longer be able to import African rodents or civets for science, education, or exhibition under the more restrictive alternative. Thus, the societal costs of disallowing importation of animals with special permits under temporary embargos would outweigh the potential cost savings associated with the time spent filing for special permits. HHS/CDC would like to solicit public comment on the value of continuing to allow importation of animals under temporary embargos for science, education, and exhibition with special permits.
B. The Regulatory Flexibility Act
Under the Regulatory Flexibility Act, as amended by the Small Business Regulatory Enforcement Fairness Act (SBREFA), agencies are required to analyze regulatory options to minimize significant economic impact of a rule on small businesses, small governmental units, and small not-for-profit organizations. HHS/CDC finds that the NPRM is not expected to change the cost of compliance for small businesses, small governmental units, or small not-for-profit organizations.
C. Paperwork Reduction Act of 1995
HHS/CDC has determined that this NPRM contains proposed information collections that are subject to review by the Office of Management and Budget (OMB) under the Paperwork Reduction Act of 1995 (PRA) (44 U.S.C. 3501-3520). A description of these proposed provisions is given below with an estimate of the annual reporting and recordkeeping burden. Included in the estimate is the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing each collection of information. Comments are invited on the following subjects.
- Whether the proposed collection of information is necessary for the proper performance of the functions of HHS/CDC, including whether the information will have practical utility.
- The accuracy of HHS/CDC’s estimate of the burden of the collection of information.
- Ways to enhance the quality, utility, and clarity of the information to be collected.
- Ways to minimize the burden of the collection of information on respondents, including by using information technology.
While HHS/CDC currently has approval to collect certain information concerning illnesses and travels under OMB Control Numbers 0920-0134 (Foreign Quarantine Regulations, expiration date 05/31/2019) and 0920-0488 (Restrictions on Interstate Travel of Persons, expiration date 05/31/2019), this NPRM is proposing updates to certain information collections within these control numbers.
In a separate information collection request accompanying this NPRM, CDC is also requesting approval to require that airlines and vessels provide certain data elements to CDC, as described in proposed 71.4 and 71.5, for the purposes of contact tracing. This information is used to locate individuals, both passengers and crewmembers, who may have been exposed to a communicable disease during travel and to provide them with appropriate public health follow-up.
CDC is taking public comment on the burden to the public outlined in the three information collection requests below.
Written comments should be received within 60 days of the publication of this NPRM. Please send written comments to Information Collection Review Office, 1600 Clifton Road NE., Atlanta, GA 30333.
Proposed Projects
(1) Foreign Quarantine Regulations (42 CFR part 71) (OMB Control No. 0920-0134)—Nonmaterial/non-substantive change—National Center for Emerging, and Zoonotic Infectious Diseases (NCEZID), Centers for Disease Control and Prevention (CDC).
(2) Restrictions on Interstate Travel of Persons (42 CFR part 70) (OMB Control No. 0920-0488)—Nonmaterial/non-substantive change—National Center for Emerging, and Zoonotic Infectious Diseases (NCEZID), Centers for Disease Control and Prevention (CDC).
(3) Airline and Vessel and Traveler Information Collection (42 CFR part 70 and 71)—New Information Collection Request—National Center for Emerging, and Zoonotic Infectious Diseases (NCEZID), Centers for Disease Control and Prevention (CDC).
Description
Section 361 of the Public Health Service (PHS) Act (42 U.S.C. 264) authorizes the Secretary of Health and Human Services to make and enforce regulations necessary to prevent the introduction, transmission, or spread of communicable diseases from foreign countries into the United States. Legislation and existing regulations governing foreign and interstate quarantine activities (42 CFR parts 70and 71) authorize quarantine officers and other personnel to inspect and undertake necessary control measures in order to protect the public health. Currently, with the exception of the CDC’s Vessel Sanitation Program, inspections are performed only on those vessels and aircraft that report illness before arriving or when illness is discovered upon arrival. Other inspection agencies assist quarantine officers in public health risk assessment and management of persons, pets, and other importations of public health importance. These practices and procedures ensure protection against the introduction and spread of communicable diseases into the United States with a minimum of recordkeeping and reporting as well as a minimum of interference with trade and travel. The information collection burden is associated with these recordkeeping and reporting requirements.
At present, HHS/CDC has approval from OMB to collect certain information and impose recordkeeping requirements related to foreign quarantine responsibilities under OMB Control Number 0920-0134(expiration 05/31/2019). The specific provisions within 42 CFR part 71that include information collection under are as follows:
42 CFR 71.21(a), (b), and (c) Radio report of death and illness.
42 CFR 71.33(c) Report of persons held in isolation or surveillance.
42 CFR 71.35 Report of death or illness on carrier during stay in port.
42 CFR 71.51 Dogs and cats.
42 CFR 71.52 Turtles, terrapins, tortoises.
42 CFR 71.56 African Rodents.
HHS/CDC has also used its authority under 42 CFR 71.32 to require importers to submit statements or documentation of non-infectiousness for those items that may constitute a public health risk if not rendered non-infectious.
Finally, HHS/CDC has approval from OMB to request from importers/filers certain data elements to identify and clear HHS/CDC regulated imports via the Automated Commercial Environment and the International Trade Data System. These HHS/CDC Partner Government Agency Message Sets are currently limited to: HHS/CDC PGA Message Set for Importing Cats and Dogs, HHS/CDC PGA Message Set for Importing African Rodents, HHS/CDC PGA Message Set for Importing African Rodent and All Family Viverridae Products.
In this NPRM, HHS/CDC is proposing 4 non-substantive changes to OMB Control Number 0920-0134 Foreign Quarantine Regulations (42 CFR part 71):
(1) Updating the definition of “ill person”, which relates to the illness reporting requirements under 42 CFR 71.21(a), (b), and (c) for airlines and vessels arriving into the United States. CDC is proposing to update the definition of “ill person” by codifying current practice with the anticipated effect of better facilitating identification of communicable diseases of concern and quarantinable communicable diseases aboard flights and maritime voyages to the United States, diseases such as measles, viral hemorrhagic fevers, active tuberculosis, and influenza caused by novel or re-emergent influenza viruses that are causing or have the potential to cause a pandemic. CDC is also proposing to include a provision to allow the Director to add new symptoms to the definition of ill person to respond to unknown communicable diseases that may emerge as future concerns.
The current definition of ill person, which applies to both airlines and maritime vessels, is anyone who:
(1) Has a temperature of 100.4 °F (or 38 °C) or greater, accompanied by a rash, glandular swelling, or jaundice, or which has persisted for more than 48 hours; or
(2) Has diarrhea, defined as the occurrence in a 24-hour period of three or more loose stools or of a greater than normal (for the person) amount of loose stools.
The proposed definition of ill person in the context of aircraft is proposed as follows:
(a) Who if onboard an aircraft:
(1) Has a fever (a measured temperature of 100.4 °F [38 °C] or greater; or feeling warm to the touch; or giving a history of feeling feverish) accompanied by one or more of the following: Skin rash, difficulty breathing, persistent cough, decreased consciousness or confusion of recent onset, new unexplained bruising or bleeding (without previous injury), persistent diarrhea, persistent vomiting (other than air sickness), headache with stiff neck, or appears obviously unwell; or
(2) Has symptoms or other indications of communicable disease, as the CDC may announce through posting of a notice in the Federal Register.
The proposed definition of ill person in the context of vessels is as follows:
(b) Who if onboard a vessel:
(1) Has a fever (a measured temperature of 100.4 °F [38 °C] or greater; or feeling warm to the touch; or giving a history of feeling feverish) accompanied by one or more of the following: Skin rash, difficulty breathing, persistent cough, decreased consciousness or confusion of recent onset, new unexplained bruising or bleeding (without previous injury), persistent vomiting (other than sea sickness), headache with stiff neck, or appears obviously unwell; or
(2) Has acute gastroenteritis, which means either diarrhea, defined as three or more episodes of loose stools in a 24 hour period or what is above normal for the individual, or vomiting accompanied by one or more of the following: one or more episodes of loose stools in a 24 hour period, abdominal cramps, headache, muscle aches, or fever (temperature of 100.4 °F [38 °C] or greater); or
(3) Has symptoms or other indications of communicable disease, as the CDC may announce through posting of a notice in the Federal Register.
The NPRM proposes to update the current definition of ill person to better focus on the signs and symptoms of communicable diseases of public health concern and quarantinable communicable diseases. The changes define an ill person in the context of the medical resources available to the operator of an airline or vessel.
CDC already requests from pilots in command of aircraft and commanders of vessels several of the symptoms included in the revised definition of ill person through publicly available guidance to airlines and vessels. Moreover, for airlines, the updated definition also better aligns with symptoms reporting guidelines published by ICAO in Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation, and the definition of “acute gastroenteritis” is used by the WHO and is currently included in reporting guidance from CDC’s Vessel Sanitation Program. Therefore, CDC does not anticipate additional burden on airlines or vessel operators to respond to these information collections.
(2) CDC is seeking a change in the title of the information collection pertaining to reports of death and illness from vessels to CDC. The current title is Radio Report of death or illness—illness reports from ships. CDC seeks a change to remove “Radio” from the title. This change reflects the fact that reports to CDC primarily via means other than radio, such as the Maritime Illness and Death Reporting System, managed by CDC’s Vessel Sanitation Program.
(3) CDC is seeking a change in the title of a specific information collection pertaining to reports of gastro-intestinal illness to CDC. CDC is updating the definition of ill person and is replacing the term “gastro-intestinal” with “acute gastroenteritis”; therefore, the title change is requested to align with the definition.
(4) CDC is seeking a change in title of respondents from “Maritime Conveyance Operator” to “Maritime Vessel Operator”” and from “Airline Commander or Operator” to “Pilot in Command”.
Table 1 below presents estimates of annual burden (in hours) associated with each reporting and recordkeeping requirement under this OMB control number, accounting for the proposed rule changes.
Description of Respondents. Respondents to this data collection include pilots in command of aircraft, maritime vessel operators, importers/filers, and travelers/general public. The nature of the response to HHS/CDC dictates which forms are completed and by whom. The total requested burden hours are 82,779.
There is no burden to respondents other than the time taken to complete the reports to CDC, maintain recordkeeping of illness aboard vessels and records of sickness or death in imported cats and dogs, as outlined in the table below. If a cat or dog is ill upon arrival, or dies prior to arrival, an exam is required, the initial exam fee may be between $100 and $200. Rabies testing on a dog that dies may be between $50 and $100. The expected number of ill or dead dogs arriving into the United States for which CDC may require an examination is estimated at less than 30 per year.
| Type of respondent | Regulatory provision or form name | Number of respondents | Number of responses per respondent | Average burden per response (in hours) | Total burden hours |
|---|---|---|---|---|---|
| Maritime Vessel Operators | 42 CFR 71.21(a) Report of illness or death from ships—Maritime Vessel Illness or Death Investigation Form/Cumulative Influenza/Influenza-Like Illness (ILI) Form/Radio report or transcribed email | 2,000 | 1 | 2/60 | 67 |
| Pilot in Command | 42 CFR 71.21 (b) Death/Illness reports from aircraft | 1,700 | 1 | 2/60 | 57 |
| Maritime Vessel Operators | 42 CFR 71.21(c) (MIDRS) Acute Gastro-Enteritis reports (24 and 4 hours before arrival) | 17,000 | 1 | 3/60 | 850 |
| Maritime Vessel Operators | 42 CFR 71.21 (c) Recordkeeping—Medical logs | 17,000 | 1 | 3/60 | 850 |
| Isolated or Quarantined individuals | 42 CFR 71.33 Report by persons in isolation or surveillance | 11 | 1 | 3/60 | 1 |
| Maritime Vessel Operators | 42 CFR 71.35 Report of death/illness during stay in port | 5 | 1 | 30/60 | 3 |
| Importer | 42 CFR 71.51(c)(1), (d)—Valid Rabies Vaccination Certificates | 245,310 | 1 | 15/60 | 61,328 |
| Importer | CDC Form 75.37 Notice To Owners And Importers Of Dogs: Requirement for Dog Confinement | 1,400 | 1 | 10/60 | 233 |
| Importer | 42 CFR 71.51(c)(i), (ii), and (iii) exemption criteria for the importation of a dog without a rabies vaccination certificate | 43,290 | 1 | 15/60 | 10,823 |
| Importer | 42 CFR 71.51(c)(2), (d) Application For Permission To Import A Dog Inadequately Against Rabies | 1400 | 1 | 15/60 | 350 |
| Importer | 42 CFR 71.51(b) (3) Dogs/cats: Record of sickness or deaths | 20 | 1 | 15/60 | 5 |
| Importer/Filer | 42 CFR 71.51_CDC Requested Data on Regulated Imports: Domestic Dogs and Cats (PGA Message Set) | 30,000 | 1 | 15/60 | 7,500 |
| Importer | 42 CFR 71.52(d) Turtle Importation Permits | 5 | 1 | 30/60 | 3 |
| Importers | 42 CFR 71.55, 42 CFR 71.32 Dead Bodies—Death certificates | 5 | 1 | 1 | 5 |
| Importer | 42 CFR 71.56 (a)(2) African Rodents—Request for exemption | 20 | 1 | 1 | 20 |
| Importer | 42 CFR 71.56(a)(iii) Appeal | 2 | 1 | 1 | 2 |
| Importer/Filer | 42 CFR 71.56 CDC Requested Data on Regulation Imports: Live African Rodents (PGA Message Set) | 60 | 1 | 15/60 | 15 |
| Importer/Filer | 42 CFR 71.32Statements or documentation of non-infectiousness | 2000 | 1 | 5/60 | 167 |
| Importer/Filer | 42 CFR 71.56, 42 CFR 71.32 CDC Requested Data on Regulated Imports: Products of African Rodents; Products of all Family Viverridae (PGA Message Set) | 2,000 | 1 | 15/60 | 500 |
| Total | 82,779 |
The estimates are based on experience to date with current recordkeeping and reporting requirements of 42 CFR part 71, with additional burden included to account for the potential for increased reports of illness during an outbreak and for reports of disease that may have been missed by airlines or vessels and are reported to CDC after travel.
Under this NPRM, CDC is also proposing a nonmaterial/non-substantive change to Restrictions on Interstate Travel of Persons (42 CFR part 70) (OMB Control No. 0920-0488). The regulations at 42 CFR part 70 are intended to prevent the interstate spread of disease, and include a requirement that the master of vessel or person in charge of conveyance to report the occurrence on board of communicable disease. Under this regulation and control number, CDC has approval to collect the following information:
- 42 CFR 70.4 Report by the master of a vessel or person in charge of conveyance of the incidence of a communicable disease occurring while in interstate travel
Through this NPRM, CDC is proposing to add the provision 70.11Report of death or illness onboard aircraft operated by airline, which specifies that the pilot in command of an aircraft operating on behalf of an airline who conducts a commercial passenger flight in interstate traffic under a regular schedule, or another designated official, shall report as soon as practicable to HHS/CDC the occurrence onboard of any deaths or ill persons among passengers or crew and take such measures as HHS/CDC may direct to prevent the potential spread of the communicable disease. HHS/CDC notes that it is not proposing changes to its existing regulatory requirement at 42 CFR 70.4, which states that the master of a vessel or person in charge of any conveyance engaged in interstate traffic on which a case or suspected case of communicable disease develops shall, as soon as practicable, notify the local health authority.
Under the NPRM, pilots in command of an aircraft, operating on behalf of an airline, that submit the ill person or death report to HHS/CDC under proposed 70.11 will not be required to also submit a report to the local health authority under current 70.4. HHS/CDC will continue to share public health information with state and local health departments through electronic disease reporting networks. It is unlikely that HHS/CDC would request follow-up reports of illnesses that are reported to the local health authorities, unless there was an urgent public health need. Therefore, CDC does not anticipate any additional burden to the respondents; however, the accounting for burden in Table 7 will add 70.11 Report of death or illness onboard aircraft operated by airline.
As a result of this proposal, CDC does not anticipate a change in total burden. CDC is instead allocating 95% of the reports of illness or death within the proposed 70.11 Report of death or illness onboard aircraft operated by airline. The remains 5% will remain within 70.4 Report by the master of a vessel or person in charge of conveyance of the incidence of a communicable disease occurring while in interstate travel, in the event that some reports are still made to State health authorities.
In addition to the requirement to report directly to HHS/CDC, HHS/CDC is proposing to include the definition of “ill person” for the purposes of illness reports to HHS/CDC in 42 CFR part 70. HHS/CDC has, as a matter of agency guidance, communicated with airlines that the same current set of required and requested signs and symptoms of disease, as well as any death, apply to domestic as well as international flights. This guidance is similar to that of the guidelines issued by ICAO under Note 1 to paragraph 8.15 of Annex 9 to the Convention on International Civil Aviation. Therefore, the new proposed definition of ill person should not affect standard practice, and no change in burden is anticipated.
Table 2 below presents estimates of annual burden (in hours) associated with each reporting and recordkeeping requirement under this OMB control number, accounting for the proposed rule changes.
Description of Respondents.
Respondents to this data collection include masters of vessels or persons in charge of conveyance and pilots in command of aircraft.
| Type of respondent | Form name | Number of respondents | Number of responses per respondent | Average burden per response (in hours) | Total burden (in hours) |
|---|---|---|---|---|---|
| Pilot in command | 42 CFR 70.11Report of death or illness onboard aircraft operated by airline | 190 | 1 | 7/60 | 22 |
| Master of vessel or person in charge of conveyance | 42 CFR 70.4Report by the master of a vessel or person in charge of conveyance of the incidence of a communicable disease occurring while in interstate travel | 10 | 1 | 7/60 | 1 |
| Total | 200 | 23 |
The total requested burden hours are 23. There is no burden to respondents other than the time taken to complete the reports. The estimates are based on experience to date with current recordkeeping and reporting requirements of 42 CFR part 70, and take into account the potential for additional burden from increased reports of illness during an outbreak and for reports of disease that may have been missed by respondents during travel and are reported to CDC by other means.
Finally, under this NPRM HHS/CDC is proposing a new information collection, Airline and Vessel and Traveler Information Collection (42 CFR part 70 and 71). This information collection request accompanies the proposed codification of issuing orders to airlines and vessel operators for the provision to CDC of airline and vessel and traveler information (aka manifests) in the event that a quarantinable communicable disease or a communicable disease of public health concern, or a death caused by a quarantinable communicable disease or communicable disease of public health concern, occurs during travel to the United States and public health follow-up is warranted. These proposed provisions are found in 42 CFR 71.4 for airlines and 71.5 for vessels.
The ordering of manifests from airlines and vessel operators arriving into the United States is an ongoing activity executed under CDC’s broad regulatory authority found at 42 CFR 71.32 Persons, carriers, and things. In order to the increase transparency with regard to CDC’s authorities and manifest order process, CDC is proposing specific regulatory provisions that outline the particular data elements CDC requires to perform contact tracing investigations. As stated in the NPRM, CDC is not mandating the collection of additional data. Only that if the airlines or maritime operators have the data elements listed in proposed 71.4 and 71.5 in their possession, they must be provided to CDC within 24 hours.
While not included in the text of this NPRM, CDC is also seeking to include two other information collections, as described in the Supporting Statement of the information collection request accompanying this NPRM.
(1) To include the collection of airline and vessel information, and passenger and crew member manifest information, from airlines and vessels engaged in interstate travel. CDC is not codifying these domestic orders in the regulation at this time.
(2) CDC is proposing to transition the Passenger Locator Form, previously approved under OMB Control Number 0920-0134 Foreign Quarantine Regulations, to this new information collection request and is proposing the ability to use the Passenger Locator Form for travelers on domestic flights.
CDC is not including burden for manifest orders for maritime vessels in the Paperwork Reduction Act section of the NPRM because CDC anticipates fewer than 10 maritime vessel manifest orders per year. Additionally, while the domestic manifest orders and transition of the Passenger Locator Form from OMB Control Number 0920-0134 into this Information Collection Request are accounted for in the Supporting Statement for Airline and Vessel and Traveler Information Collection (42 CFR part 70 and 71), they are not included here, as this NPRM is only codifying current practice with regard to manifest orders related to international flights arriving into the United States. Please see the accompanying Supporting Statement for further information on these additional information collections.
Table 3 below presents estimates of annual burden (in hours) associated with each reporting and recordkeeping requirement under this OMB control number, accounting for the proposed rule changes.
Description of Respondents.
Respondents to this data collection include the Airline Medical Officer or Equivalent and a Computer and Information Systems Manager.
| Type of respondent | Form name | Number of respondents | Number of responses per respondent | Average burden per response (in hours) | Total burden (in hours) |
|---|---|---|---|---|---|
| Airline Medical Officer or Equivalent/Computer and Information Systems Manager | International TB Manifest Template | 67 | 1 | 360/60 | 402 |
| Airline Medical Officer or Equivalent/Computer and Information Systems Manager | International Non-TB Manifest Template. | 29 | 1 | 360/60 | 174 |
| Total | 96 | 576 |
The total requested burden hours included in this NPRM for proposed are 576. There is no burden to respondents other than the time taken to complete the manifest information and send to CDC. The estimates are based on experience to date with current manifest order process.
D. National Environmental Policy Act (NEPA)
HHS/CDC has determined that the proposed amendments to 42 CFR part 70 and 71 will not have a significant impact on the human environment. Therefore, neither an environmental assessment nor an environmental impact statement is needed.
E. EO 12988: Civil Justice Reform
HHS/CDC has reviewed this rule under Executive Order 12988 on Civil Justice Reform and determines that this NPRM meets the standard in the Executive Order.
F. EO 13132: Federalism
Under Executive Order 13132, if the rulemaking would limit or preempt State authorities, then a Federalism analysis is required. The agency must consult with State and local officials to determine whether the rule would have a substantial direct effect on State or local Governments, as well as whether it would either preempt State law or impose a substantial direct cost of compliance on them.
HHS/CDC has determined that this NPRM will not have sufficient Federalism implications to warrant the preparation of a Federalism summary impact statement.
G. Plain Language Act of 2010
Under 63 FR 31883 (June 10, 1998), Executive Departments and Agencies are required to use plain language in all proposed and final rules. HHS/CDC has attempted to use plain language in this rulemaking to make our intentions and rationale clear and requests input from the public in this regard.
List of Subjects in42 CFR Parts 70 and 71Back to Top
- Apprehension
- Communicable diseases
- Conditional release
- CDC
- Ill person
- Isolation
- Non-invasive
- Public health emergency
- Public health prevention measures
- Qualifying stage
- Quarantine
- Quarantinable Communicable Disease
For the reasons discussed in the preamble, we propose to amend 42 CFR parts 70 and 71 as follows:
PART 70—INTERSTATE QUARANTINEBack to Top
1.The authority citation for part 70 continues to read as follows:
2.Amend § 70.1 by adding, in alphabetical order the definitions of “Agreement,” “Airlines,” “Apprehension,” “Communicable stage,” “Conditional release,” “Contaminated environment,” “Conveyance,” “Electronic or Internet-based monitoring,” “Ill person,” “Incubation Period,” “Master or operator,” “Medical examination,” “Medical representative,” “Medical reviewer,” “Non-invasive,” “Precommunicable stage,” “Public health emergency,”: Public health prevention measures,” “Qualifying stage,” and “Reasonably believed to be infected, as applied to an individual” to read as follows:
§ 70.1 General definitions.
Agreement means an agreement entered into between the CDC and an individual expressing a voluntary agreement between the parties that the individual will observe public health measures authorized under this part, as the CDC considers reasonably necessary to protect the public’s health, including quarantine, isolation, conditional release, medical examination, hospitalization, vaccination, and treatment.
Airline(s) means any air carrier(s) or foreign air carrier(s) providing air transportation, including scheduled or public charter passenger operations operating in air commerce within the United States, as these terms are defined in 49 U.S.C. 40102, (a)(2), (a)(3), (a)(5), and (a)(21).
Apprehension means the temporary taking into custody of an individual or group for purposes of determining whether Federal quarantine, isolation, or conditional release is warranted.
* * * * *
Communicable stage means the stage during which an infectious agent may be transmitted either directly or indirectly from an infected individual to another individual.
Conditional release means surveillance as defined under 42 CFR 71.1 and includes public health supervision through in-person visits by a health official or designee, telephone, or through electronic or internet-based monitoring.
Contaminated environment means the presence of an infectious agent on a surface, including on inanimate articles, or in a substance, including food, water, or in the air.
Conveyance means an aircraft, train, road vehicle, vessel (as defined in this section) or other means of transport, including military.
* * * * *
Electronic or Internet-based monitoring means mechanisms or technologies allowing for the temporary public health supervision of an individual under conditional release and may include electronic mail, SMS texts, video conference or webcam technologies, integrated voice-response systems, entry of information into a web-based forum, wearable tracking technologies, and other mechanisms or technologies as determined by the Director or supervising health authority.
Ill person means an individual who:
(1) Has a fever (a measured temperature of 100.4 °F [38 °C] or greater, or feels warm to the touch, or gives a history of feeling feverish) accompanied by one or more of the following: Skin rash, difficulty breathing, persistent cough, decreased consciousness or confusion of recent onset, new unexplained bruising or bleeding (without previous injury), persistent diarrhea, persistent vomiting (other than air sickness), headache with stiff neck, appears obviously unwell; or
(2) Has a fever that has persisted for more than 48 hours; or
(3) Has symptoms or other indications of communicable disease, as the CDC may announce through posting of a notice in the Federal Register.
Incubation period means the time from the moment of exposure to an infectious agent that causes a communicable disease until signs and symptoms of the communicable disease appear in the individual. For a quarantinable communicable disease, incubation period means the precommunicable stage.
Indigent means an individual whose annual family income is below 150% of the applicable poverty guidelines updated periodically in the Federal Register by the U.S. Department of Health and Human Services under the authority of 42 U.S.C. 9902(2) or, if no income is earned, liquid assets totaling less than 15% of the applicable poverty guidelines.
* * * * *
Master or operator with respect to a vessel, means the sea crew member with responsibility for vessel operation and navigation, or a similar individual with responsibility for a conveyance. Consistent with the definition of “operate” in 14 CFR 1.1, “operator” means, with respect to aircraft, any person who uses, causes to use or authorizes to use an aircraft, for the purpose (except as provided in 14 CFR 91.13) of air navigation including the piloting of an aircraft, with or without the right of legal control (as owner, lessee, or otherwise).
Medical examination means the assessment of an individual by an authorized health worker to determine the individual’s health status and potential public health risk to others and may include the taking of a medical history, a physical examination, and collection of human biological samples for laboratory testing as may be needed to diagnose or confirm the presence or extent of infection with a quarantinable communicable disease.
Medical representative means a physician, nurse practitioner, or similar medical professional qualified in the diagnosis and treatment of infectious diseases who is appointed by the HHS Secretary or CDC Director and may include an HHS or CDC employee, to assist an indigent individual under Federal quarantine, isolation, or conditional release with a medical review under this part.
Medical reviewer means a physician, nurse practitioner, or similar medical professional qualified in the diagnosis and treatment of infectious diseases who is appointed by the HHS Secretary or CDC Director to conduct medical reviews under this part and may include an HHS or CDC employee, provided that the employee differs from the CDC official who issued the Federal order for quarantine, isolation, or conditional release.
Non-invasive means procedures conducted by an authorized health worker or another individual with suitable training and includes the physical examination of the ear, nose, and mouth; temperature assessments using an ear, oral, cutaneous, or noncontact thermometer, or thermal imaging; auscultation; external palpation; external measurement of blood pressure; and other procedures not involving the puncture or incision of the skin or insertion of an instrument or foreign material into the body or a body cavity excluding the ear, nose and mouth.
* * * * *
Precommunicable stage means the stage beginning upon an individual’s earliest opportunity for exposure to an infectious agent and ending upon the individual entering or reentering the communicable stage of the disease or, if the individual does not enter the communicable stage, the latest date at which the individual could reasonably be expected to have the potential to enter or reenter the communicable stage.
Public health emergency as used in this part means
(1) Any communicable disease event as determined by the Director with either documented or significant potential for regional, national, or international communicable disease spread or that is highly likely to cause death or serious illness if not properly controlled; or
(2) Any communicable disease event described in a declaration by the Secretary pursuant to § 319(a) of the Public Health Service Act (42 U.S.C. 247d (a)); or
(3) Any communicable disease event the occurrence of which is notified to the World Health Organization, in accordance with Articles 6 and 7 of the International Health Regulations, as one that may constitute a Public Health Emergency of International Concern; or
(4) Any communicable disease event the occurrence of which is determined by the Director-General of the World Health Organization, in accordance with Article 12 of the International Health Regulations, to constitute a Public Health Emergency of International Concern; or
(5) Any communicable disease event for which the Director-General of the World Health Organization, in accordance with Articles 15 or 16 of the International Health Regulations, has issued temporary or standing recommendations for purposes of preventing or promptly detecting the occurrence or reoccurrence of the communicable disease.
Public health prevention measures means the assessment of an individual through non-invasive procedures and other means, such as observation, questioning, review of travel documents, records review, and other non-invasive means, to determine the individual’s health status and potential public health risk to others.
Qualifying stage is statutorily defined (42 U.S.C. 264(d)(2)) to mean:
(1) The communicable stage of a quarantinable communicable disease; or
(2) The precommunicable stage of the quarantinable communicable disease, but only if the quarantinable communicable disease would be likely to cause a public health emergency if transmitted to other individuals.
* * * * *
Reasonably believed to be infected, as applied to an individual, means specific articulable facts upon which a public health officer could reasonably draw the inference that an individual has been exposed, either directly or indirectly, to the infectious agent that causes a quarantinable communicable disease, as through contact with an infected person or an infected person’s bodily fluids, a contaminated environment, or through an intermediate host or vector, and that as a consequence of the exposure, the individual is or may be harboring in the body the infectious agent of that quarantinable communicable disease.
* * * * *
3.Revise § 70.5 to read as follows:
§ 70.5 Requirements relating to travelers under a Federal order of isolation, quarantine, or conditional release.
(a) The following provisions are applicable to any individual under a Federal order, or agreement, of isolation, quarantine, or conditional release with regard to a quarantinable communicable disease or to any individual meeting the requirements of subparagraph (d) or (e) of this section:
(1) No such individual shall travel in interstate traffic or from one state or U.S. territory to another without a written travel permit issued by HHS/CDC.
(2) Requests for a travel permit must state the reasons why the travel is being requested, mode of transportation, the places or individuals to be visited, the precautions, if any, to be taken to prevent the potential transmission or spread of the communicable disease, and other information as determined necessary by the CDC to assess the individual’s health condition and potential for communicable disease spread to others.
(3) The CDC will consider all requests for a permit and, taking into consideration the risk of introduction, transmission, or spread of the communicable disease, may condition the permit upon compliance with such precautionary measures as the CDC shall prescribe.
(4) An individual to whom a permit has been issued shall retain it in his/her possession throughout the course of his/her authorized travel and comply with all conditions prescribed therein, including presentation of the permit to the operators of conveyances, as required by its terms.
(5) An individual who has had his/her request for a permit denied, or who has had a travel permit suspended or revoked, may submit a written appeal to the Director. The appeal must be in writing, state the factual basis for the appeal, and be submitted to the Director within 10 calendar days of the denial, suspension, or revocation of the permit. The CDC will promptly issue a written response to the appeal, which shall constitute final agency action.
(b) The operator of any conveyance operating in interstate traffic shall not:
(1) Accept for transportation any individual whom the operator knows, or reasonably should know, to be under a Federal order or agreement of isolation, quarantine, or conditional release, unless such an individual presents a permit issued by the CDC authorizing such travel;
(2) Transport any individual whom the operator knows, or reasonably should know, to be under a Federal order or agreement of isolation, quarantine, or conditional release in violation of any of the terms or conditions prescribed in the travel permit issued by the CDC.
(c) Whenever a conveyance operating in interstate traffic transports an individual under a Federal order, travel permit, or agreement of isolation, quarantine, or conditional release, CDC may require that the operator of the conveyance submit the conveyance to inspection, sanitary measures, and other measures, as the CDC deems necessary to prevent the possible spread of communicable disease.
(d) CDC may additionally apply the provisions in paragraphs (a) through (c) of this section upon the request of a state or local health authority of jurisdiction or whenever the Director makes a determination under 42 CFR 70.2 that is based on the existence of inadequate local control such measures are needed to prevent the spread of any of the communicable diseases from such State or U.S. territory to any other State or U.S. territory.
(e) CDC may additionally apply the provisions in paragraphs (a) through (c) of this section to individuals under a state or local order, or written agreement, for quarantine, isolation, or conditional release and to conveyances that may transport such individuals, upon the request of a state or local health authority of jurisdiction or whenever the Director makes a determination of inadequate local control under 42 CFR 70.2.
(f) The CDC may exempt individuals and non-public conveyances, such as ambulances, air ambulance flights, or private vehicles, from the requirements of this section.
4.Revise § 70.6 to read as follows:
§ 70.6 Apprehension and detention of persons with quarantinable communicable diseases.
CDC may authorize the apprehension, medical examination, quarantine, isolation, or conditional release of any individual for the purpose of preventing the introduction, transmission, and spread of quarantinable communicable diseases, as specified by Executive Order, based upon a finding that:
(a) The individual is reasonably believed to be infected with a quarantinable communicable disease in a qualifying stage and is moving or about to move from a state into another state; or
(b) The individual is reasonably believed to be infected with a quarantinable communicable disease in a qualifying stage and constitutes a probable source of infection to other individuals who may be moving from a state into another state.
5.Add §§ 70.10 through 70.19 to read as follows:
§ 70.10 Public health prevention measures to detect communicable disease.
(a) The CDC may conduct public health prevention measures at U.S. airports, seaports, railway stations, bus terminals, and other locations where individuals may gather to engage in interstate travel, through non-invasive procedures determined appropriate by the CDC to detect the presence of communicable diseases.
(b) As part of the public health prevention measures, CDC may require individuals to provide contact information such as U.S. and foreign addresses, telephone numbers, email addresses, and other contact information, as well as information concerning their intended destination, health status, and travel history.
§ 70.11 Report of death or illness onboard aircraft operated by airline.
(a) The pilot in command of an aircraft operated on behalf of an airline who is conducting a commercial passenger flight in interstate traffic under a regular schedule shall report as soon as practicable to the CDC the occurrence onboard of any deaths or the presence of ill persons among passengers or crew and take such measures as the CDC may direct to prevent the potential spread of the communicable disease, provided that such measures do not affect the airworthiness of the aircraft or the safety of flight operations.
(b) The pilot in command of an aircraft operated on behalf of an airline who reports in accordance with paragraph (a) shall be deemed to satisfy the reporting obligation under42 CFR 70.4.
§ 70.12 Medical examinations.
(a) The CDC may require an individual to undergo a medical examination as part of a Federal order for quarantine, isolation, or conditional release for a quarantinable communicable disease.
(b) The CDC shall promptly arrange for the medical examination to be conducted when one is required under this section.
(c) As part of the medical examination, the CDC may require an individual to provide information and undergo such testing as may be reasonably necessary to diagnose or confirm the presence or extent of infection with a quarantinable communicable disease.
(d) Individuals reasonably believed to be infected based on the results of a medical examination may be isolated, or if such results are inconclusive or unavailable, individuals may be quarantined or conditionally released in accordance with this part.
§ 70.13 Payment for care and treatment.
(a) The CDC may authorize payment for the care and treatment of individuals subject to medical examination, quarantine, isolation, and conditional release, subject to paragraphs (b) through (h) of this section.
(b) Payment for care and treatment shall be in the CDC’s sole discretion and subject to the availability of appropriations.
(c) Payment shall be secondary to the obligation of the United States or any third-party (i.e., any state or local governmental entity, private insurance carrier, or employer), under any other law or contractual agreement, to pay for such care and treatment, and shall be paid by the CDC only after all third-party payers have made payment in satisfaction of their obligations.
(d) Payment may include costs for providing ambulance or other medical transportation when such services are deemed necessary by the CDC for the individual’s care and treatment.
(e) Payment shall be limited to those amounts the hospital, medical facility, or medical transportation service would customarily bill the Medicare system using the International Classification of Diseases, Clinical Modification (ICD-CM), and relevant regulations promulgated by the Centers for Medicare and Medicaid Services in existence at the time of billing.
(f) For quarantinable communicable diseases, payment shall be limited to costs for services and items reasonable and necessary for the care and treatment of the individual or group for the time period beginning when the CDC refers the individual or group to the hospital or medical facility and ends when, as determined by the CDC, the period of apprehension, quarantine, isolation, or conditional release expires.
(g) For diseases other than those described in paragraph (f) of this section, such payment shall be limited to costs for services and items reasonable and necessary for care and treatment of the individual for the time period that begins when the CDC refers the individual to the hospital or medical facility and ends when the individual’s condition is diagnosed, as determined by the CDC, as an illness other than a quarantinable communicable disease.
(h) For ambulance or other medical transportation, payment shall be limited to the costs for such services and other items reasonable and necessary for the individual’s safe medical transport.
§ 70.14 Requirements relating to the issuance of a Federal order for quarantine, isolation, or conditional release.
(a) A Federal order authorizing quarantine, isolation, or conditional release shall be in writing, signed by a CDC authorizing official, and contain the following information:
(1) The identity of the individual or group subject to the order;
(2) The location of the quarantine or isolation or, in the case of conditional release, the entity to who and means by which the individual shall report for public health supervision;
(3) An explanation of the factual basis underlying the CDC’s reasonable belief that the individual is in the qualifying stage of a quarantinable communicable disease;
(4) An explanation of the factual basis underlying the CDC’s reasonable belief that the individual is moving or about to move from one state into another or constitutes a probable source of infection to others who may be moving from one state into another;
(5) An explanation of the process for reassessment and medical review of the Federal order pursuant to this part; and
(6) An explanation of the criminal penalties for violating a Federal order of quarantine, isolation, or conditional release.
(b) A Federal order authorizing quarantine, isolation, or conditional release shall be promptly served on the individual, except that the Federal order may be published or posted in a conspicuous location if the Federal order is applicable to a group of individuals and individual service would be impracticable.
§ 70.15 Mandatory reassessment of a Federal order for quarantine, isolation, or conditional release.
(a) The CDC shall reassess the need to continue the quarantine, isolation, or conditional release of an individual no later than 72 hours after the service of the Federal order.
(b) As part of the reassessment, the CDC shall review all records considered in issuing the Federal order, including travel records, records evidencing exposure or infection with a quarantinable communicable disease, as well as any relevant new information.
(c) As part of the reassessment, and where applicable, the CDC shall consider whether less restrictive alternatives would adequately serve to protect the public health.
(d) At the conclusion of the reassessment, the CDC shall promptly issue a written Federal order directing that the quarantine, isolation, or conditional release be continued, modified, or rescinded.
(e) In the event that the CDC directs that the quarantine, isolation, or conditional release be continued or modified, the written Federal order shall explain the process for requesting a medical review under this part.
(f) The CDC’s written Federal order shall be promptly served on the individual, except that the Federal order may be served by publication or by posting in a conspicuous location if the Federal order is applicable to a group of individuals and individual service would be impracticable.
§ 70.16 Medical review of a Federal order for quarantine, isolation, or conditional release.
(a) The CDC shall, as soon as practicable, arrange for a medical review upon a request by an individual under Federal quarantine, isolation, or conditional release.
(b) A request for a medical review may only occur after the CDC’s mandatory reassessment under § 70.15 and following the issuance of a Federal order continuing or modifying the quarantine, isolation, or conditional release.
(c) The medical review shall be for the purpose of ascertaining whether the CDC has a reasonable belief that the individual is infected with a quarantinable communicable disease in a qualifying stage.
(d) The CDC shall notify the individual in writing of the time and place of the medical review.
(e) The CDC shall designate a medical reviewer to review the medical or other evidence presented at the review, make medical or other findings of fact, and issue a recommendation concerning whether the Federal order for quarantine, isolation, or conditional release should be rescinded, continued, or modified.
(f) The individual under Federal quarantine, isolation, or conditional release may authorize a representative at his or her own expense to submit medical or other evidence and, in the medical reviewer’s discretion, be allowed to present a reasonable number of medical experts. The CDC shall appoint a medical representative at its own expense to assist the individual for purposes of the medical review upon a request and certification, under penalty of perjury, by that individual that he or she is indigent and cannot afford a medical representative.
(g) Prior to the convening of the review, the individual or his/her authorized representative shall be provided a reasonable opportunity, to examine the available medical and other records involved in the medical review that pertain to that individual.
(h) The CDC shall take such measures that it determines to be reasonably necessary to allow an individual under Federal quarantine or isolation to communicate with an authorized representative in such a manner as to prevent the possible spread of the quarantinable communicable disease.
(i) The medical reviewer may order a medical examination of an individual when, in the medical reviewer’s professional judgment, such an examination would assist in assessing the individual’s medical condition.
(j) As part of the review, and where applicable, the medical reviewer shall consider and accept into the record evidence concerning whether less restrictive alternatives would adequately serve to protect public health.
(k) In the medical reviewer’s discretion, the review may be conducted through written submission, by telephone, or through any other means that the medical reviewer determines to be acceptable.
(l) At the conclusion of the review, the medical reviewer shall, based upon his or her review of the facts and other evidence made available during the medical review, issue a written report to the Director as to whether, in the medical reviewer’s professional judgment, the Federal quarantine, isolation, or conditional release should be rescinded, continued, or modified. The written report shall be served on the individual and the individual’s authorized representative.
(m) The Director shall, as soon as practicable, review the written report and any objections that may be submitted by the individual or the individual’s authorized representative that contest the findings and recommendation contained in the medical reviewer’s written report. Upon conclusion of the review, the Director shall promptly issue a written Federal order directing that the quarantine, isolation, or conditional release be continued, modified, or rescinded. In the event that the Director continues or modifies the Federal quarantine, isolation, or conditional release, the Director’s written order shall include a statement that the individual may request that the CDC rescind the Federal quarantine, isolation, or conditional release, but based only on a showing of significant, new or changed facts or medical evidence that raise a genuine issue as to whether the individual should continue to be subject to Federal quarantine, isolation, or conditional release. The written Federal order shall be promptly served on the individual and the individual’s authorized representative, except that the Federal order may be served by publication or by posting in a conspicuous location if applicable to a group of individuals and individual service would be impracticable.
(n) The Director’s written order shall not constitute final agency action until it has been served on the individual and the individual’s authorized representative, or alternatively, if applicable to a group of individuals and individual service would be impracticable, it is published or posted.
(o) The Director may order the consolidation of one or more medical reviews if the number of individuals or other factors makes the holding of individual medical reviews impracticable.
(p) The CDC may issue additional instructions as may be necessary or desirable governing the conduct of medical reviews.
§ 70.17 Administrative records relating to Federal quarantine, isolation, or conditional release.
(a) The administrative record of an individual under Federal quarantine, isolation, or conditional release shall, where applicable, consist of the following:
(1) The Federal order authorizing quarantine, isolation, or conditional release, including any subsequent Federal orders continuing or modifying the quarantine, isolation or conditional release;
(2) Records of any available medical, laboratory, or other epidemiologic information that are in the agency’s possession and that were considered in issuing the Federal quarantine, isolation, or conditional release order, or any subsequent Federal orders;
(3) Records submitted by the individual under quarantine, isolation, or conditional release, or by an authorized representative, as part of a request for rescission of the Federal quarantine, isolation, or conditional release or as part of a medical review;
(4) The written findings and report of the medical reviewer, including any transcripts of the medical review and any written objections submitted by the individual under Federal quarantine, isolation, or conditional release, or by an authorized representative;
(5) Any agreements entered into between the CDC and the individual.
(b) An individual subject to a Federal public health order will upon request be served with a copy of his or her own administrative record in its entirety.
§ 70.18 Agreements.
CDC may enter into an agreement with an individual, upon such terms as the CDC considers to be reasonably necessary, indicating that the individual consents to any of the public health measures authorized under this part, including quarantine, isolation, conditional release, medical examination, hospitalization, vaccination, and treatment; provided that the individual’s consent shall not be considered as a prerequisite to the exercise of any authority under this part.
§ 70.19 Penalties.
(a) Persons in violation of this part are subject to a fine of no more than $100,000 if the violation does not result in a death or one year in jail, or both, or a fine of no more than $250,000 if the violation results in a death or one year in jail, or both, or as otherwise provided by law.
(b) Violations by organizations are subject to a fine of no more than $200,000 per event if the violation does not result in a death or $500,000 per event if the violation results in a death or as otherwise provided by law.
PART 71—FOREIGN QUARANTINEBack to Top
6.The authority citation for part 71 continues to read as follows:
7.Amend § 71.1 by adding, in alphabetical order the definitions of “Agreement,” “Airlines,” “Apprehension,” “Commander,” “Conditional release,” “Contaminated environment,” “Electronic or Internet-based monitoring,” “Ill person,” “Indigent,” “Master or operator,” “Medical examination,” “Medical representative,” “Medical reviewer,” “Non-invasive,” and “Public health prevention measures,” to read as follows:
§ 71.1 General Definitions
* * * * *
(b) * * *
Agreement means an agreement entered into between the CDC and an individual expressing a voluntary agreement between the parties that the individual will observe public health measures authorized under this part, as the CDC considers reasonably necessary to protect the public’s health, including quarantine, isolation, conditional release, medical examination, hospitalization, vaccination, and treatment.
Airline(s) means any air carrier(s) or foreign air carrier(s) providing air transportation or foreign air transportation, respectively, including scheduled or public charter passenger operations operating in air commerce, as these terms are defined in 49 U.S.C. 40102,(a)(2), (a)(3), (a)(5),(a)(21), and (a)(23).
Apprehension means the temporary taking into custody of an individual or group for purposes of determining whether quarantine, isolation, or conditional release is warranted.
* * * * *
Commander means the pilot in command of an aircraft as defined in 14 CFR 1.1.
* * * * *
Conditional release means surveillance as defined under this part and includes public health supervision through in-person visits by a health official or designee, telephone, or through any electronic or internet-based means as determined by the CDC.
Contaminated environment means the presence of an infectious agent on a surface, including on inanimate articles, or in a substance, including food, water, or in the air.
* * * * *
Electronic or internet-based monitoring means mechanisms or technologies allowing for the temporary public health supervision of an individual under conditional release and may include electronic mail, SMS texts, video conference or webcam technologies, integrated voice-response systems, entry of information into a web-based forum, wearable tracking technologies, and other mechanisms or technologies as determined by the CDC.
Ill person means an individual:
(1) Who if onboard an aircraft:
(i) Has a fever (a measured temperature of 100.4 °F [38°C] or greater, or feels warm to the touch, or gives a history of feeling feverish) accompanied by one or more of the following: Skin rash, difficulty breathing, persistent cough, decreased consciousness or confusion of recent onset, new unexplained bruising or bleeding (without previous injury), persistent diarrhea, persistent vomiting (other than air sickness), headache with stiff neck, appears obviously unwell; or
(ii) Fever that has persisted for more than 48 hours; or
(iii) Has symptoms or other indications of communicable disease, as the CDC may announce through posting of a notice in the Federal Register.
(2) Who if onboard a vessel:
(i) Has a fever (a measured temperature of 100.4 °F [38°C] or greater; or feels warm to the touch; or gives a history of feeling feverish) accompanied by one or more of the following: Skin rash, difficulty breathing or suspected or confirmed pneumonia, persistent cough or cough with bloody sputum, decreased consciousness or confusion of recent onset, new unexplained bruising or bleeding (without previous injury), persistent vomiting (other than sea sickness), headache with stiff neck; or
(ii) Has diarrhea, defined as the occurrence in a 24-hour period of three or more loose stools or of a greater than normal (for the person) amount of loose stools; or
(iii) Has symptoms or other indications of communicable disease, as the CDC may announce through posting of a notice in the Federal Register.
Indigent means an individual whose annual family income is below 150% of the applicable poverty guidelines updated periodically in the Federal Register by the U.S. Department of Health and Human Services under the authority of 42 U.S.C. 9902(2) or, if no income is earned, liquid assets totaling less than 15% of the applicable poverty guidelines.
* * * * *
Master or Operator with respect to a vessel, means the sea crew member with responsibility for vessel operation and navigation, or a similar individual with responsibility for a conveyance. Consistent with the definition of “operate” in 14 CFR 1.1, “operator” means, with respect to aircraft, any person who uses, causes to use or authorizes to use aircraft, for the purpose (except as provided in 14 CFR 91.13) of air navigation including the piloting of aircraft, with or without the right of legal control (as owner, lessee, or otherwise).
Medical examination means the assessment of an individual by an authorized health worker to determine the individual’s health status and potential public health risk to others and may include the taking of a medical history, a physical examination, and collection of human biological samples for laboratory testing as may be needed to diagnose or confirm the presence or extent of infection with a quarantinable communicable disease.
Medical representative means a physician, nurse practitioner, or similar medical professional qualified in the diagnosis and treatment of infectious diseases who is appointed by the HHS Secretary or CDC Director and may include an HHS or CDC employee, to assist an indigent individual under Federal quarantine, isolation, or conditional release with a medical review under this part.
Medical reviewer means a physician, nurse practitioner, or similar medical professional qualified in the diagnosis and treatment of infectious diseases who is appointed by the HHS Secretary or CDC Director to conduct medical reviews under this part and may include an HHS or CDC employee, provided that the employee differs from the CDC official who issued the Federal order for quarantine, isolation, or conditional release.
* * * * *
Non-invasive means procedures conducted by an authorized health worker or another individual with suitable training and includes the physical examination of the ear, nose, and mouth; temperature assessments using an ear, oral, cutaneous, or noncontact thermometer, or thermal imaging; auscultation; external palpation; external measurement of blood pressure; and other procedures not involving the puncture or incision of the skin or insertion of an instrument or foreign material into the body or a body cavity excluding the ear, nose and mouth.
* * * * *
Public health prevention measures means the assessment of an individual through non-invasive procedures and other means, such as observation, questioning, review of travel documents, records review, and other non-invasive means, to determine the individual’s health status and potential public health risk to others.
* * * * *
8.Revise § 71.2 to read as follows:
§ 71.2 Penalties.
(a) Persons in violation of this part are subject to a fine of no more than $100,000 if the violation does not result in a death or one year in jail, or both, or a fine of no more than $250,000 if the violation results in a death or one year in jail, or both, or as otherwise provided by law.
(b) Violations by organizations are subject to a fine of no more than $200,000 per event if the violation does not result in a death or $500,000 per event if the violation results in a death or as otherwise provided by law.
9.Add § 71.4 to read as follows:
§ 71.4 Requirements relating to collection, storage and transmission of airline passenger, crew and flight information for public health purposes
(a) Any airline with a flight arriving into the United States, including any intermediate stops between the flight’s origin and final destination, shall make the data elements in paragraph (b) of this section available to the CDC for passengers or crew who, as determined by the CDC, may be at risk of exposure to a communicable disease, to the extent that such data are already available and maintained by the airline, within 24 hours of an order by the CDC and in a format available and acceptable to both the airline and the CDC.
(b) The data elements referred to in paragraph (a) of this section include:
(1) Full name (last, first, and, if available, middle or others);
(2) Date of birth;
(3) Sex;
(4) Country of residence;
(5) If a passport is required: passport number, passport country of issuance, and passport expiration date;
(6) If a travel document other than a passport is required: Travel document type, travel document number, travel document country of issuance and travel document expiration date;
(7) Address while in the United States (number and street, city, state, and zip code), except that U.S. citizens and lawful permanent residents will provide address of permanent residence in the U.S.(number and street, city, state, and zip code);
(8) Primary contact phone number to include country code;
(9) Secondary contact phone number to include country code;
(10) Email address;
(11) Airline name;
(12) Flight number;
(13) City of departure;
(14) Departure date and time;
(15) City of arrival;
(16) Arrival date and time; and
(17) Seat number.
10.Add § 71.5 to read as follows:
§ 71.5 Requirements relating to collection, storage and transmission of vessel passenger, crew, and voyage information for public health purposes
(a) The operator of any vessel carrying 13 or more passengers (excluding crew) and, which is not a ferry as defined under 46 U.S.C. 2101 and U.S. Coast Guard (USCG) regulations (46 CFR 2.10-25), shall make the data elements in paragraph (b) available to the CDC for passengers or crew who, as determined by the CDC, may be at risk of exposure to a communicable disease, to the extent that such data are already in the operator’s possession, within 24 hours of an order by the CDC and in a format available and acceptable to both the operator and the CDC.
(b) The data elements referred to in paragraph (a)of this section include:
(1) Full name (last, first, and, if available middle or others);
(2) Date of birth;
(3) Sex;
(4) Country of residence;
(5) If a passport is required: passport number; passport country of issuance, and passport expiration date;
(6) If a travel document other than a passport is required: Travel document type, travel document number, travel document country of issuance and travel document expiration date;
(7) Address while in the United States (number and street, city, state, and zip code), except that U.S. citizens and lawful permanent residents will provide address of permanent residence in the United States (number and street, city, state, and zip code; as applicable);
(8) Primary contact phone number to include country code;
(9) Secondary contact phone number to include country code;
(10) Email address;
(11) Vessel operator;
(12) Vessel name;
(13) Voyage number;
(14) Embarkation port and date;
(15) Disembarkation port and date;
(16) All port stops; and
(17) Cabin number.
11.Add § 71.20 to read as follows:
§ 71.20 Public health prevention measures to detect communicable disease.
(a) The CDC may conduct public health prevention measures, at U.S. ports of entry or other locations, through non-invasive procedures as defined in 42 CFR 71.1 to detect the potential presence of communicable diseases.
(b) As part of the public health prevention measures, CDC may require individuals to provide contact information such as U.S. and foreign addresses, telephone numbers, email addresses, and other contact information, as well as information concerning their intended destination, health status, and travel history.
12.Add §§ 71.29 and 71.30 to read as follows:
§ 71.29 Administrative records relating to quarantine, isolation, or conditional release.
(a) The administrative record of an individual under quarantine, isolation, or conditional release shall, where applicable, consist of the following:
(1) The Federal order authorizing quarantine, isolation, or conditional release, including any subsequent Federal orders continuing or modifying the quarantine, isolation or conditional release;
(2) Records of any available medical, laboratory, or other epidemiologic information that are in the agency’s possession and that were considered in issuing the Federal quarantine, isolation, or conditional release order, or any subsequent Federal orders;
(3) Records submitted by the individual under quarantine, isolation, or conditional release, or by an authorized representative, as part of a request for rescission of the quarantine, isolation, or conditional release or as part of a medical review;
(4) The written findings and report of the medical reviewer, including any transcripts of the medical review and any written objections submitted by the individual under Federal quarantine, isolation, or conditional release, or by an authorized representative;
(5) Any agreements entered into between the CDC and the individual.
(b) An individual subject to a Federal public health order will upon request be served with a copy of his or her own administrative record in its entirety.
§ 71.30 Payment for care and treatment.
(a) The CDC may authorize payment for the care and treatment of individuals subject to medical examination, quarantine, isolation, and conditional release, subject to paragraphs (b) through (h) of this section.
(b) Payment for care and treatment shall be in the CDC’s sole discretion and subject to the availability of appropriations.
(c) Payment shall be secondary to the obligation of the United States or any third-party (including any state or local governmental entity, private insurance carrier, or employer), under any other law or contractual agreement, to pay for such care and treatment, and shall be paid by the CDC only after all third-party payers have made payment in satisfaction of their obligations.
(d) Payment may include costs for providing ambulance or other medical transportation when such services are deemed necessary by the CDC for the individual’s care and treatment.
(e) Payment shall be limited to those amounts the hospital, medical facility, or medical transportation service would customarily bill the Medicare system using the International Classification of Diseases, Clinical Modification (ICD-CM), and relevant regulations promulgated by the Centers for Medicare and Medicaid Services in existence at the time of billing.
(f) For quarantinable communicable diseases, payment shall be limited to costs for services and items reasonable and necessary for the care and treatment of the individual for the time period beginning when the CDC refers the individual to the hospital or medical facility and ends when, as determined by the CDC, the period of apprehension, quarantine, isolation, or conditional release expires.
(g) For diseases other than those described in paragraph (f) of this section, such payment shall be limited to costs for services and items reasonable and necessary for care and treatment of the individual for the time period that begins when the CDC refers the individual to the hospital or medical facility and ends when the individual’s condition is diagnosed, as determined by the CDC, as an illness other than a quarantinable communicable disease.
(h) For ambulance or other medical transportation, payment shall be limited to the costs for such services and other items reasonable and necessary for the safe medical transport of the individual.
13.Amend § 71.33 by revising paragraph (c) to read as follows:
§ 71.33 Persons: Isolation and surveillance.
* * * * *
(c) Every person who is placed under surveillance by authority of this subpart shall, during the period of surveillance:
(1) Give information relative to his/her health and his/her intended destination and submit to surveillance, including electronic and internet-based monitoring as required by the CDC or by the state or local health department having jurisdiction over the areas to be visited, and report for such medical examinations as may be required.
(2) Inform the CDC prior to departing the United States or prior to traveling to any address other than that stated as the intended destination.
* * * * *
14.Add §§ 71.36 through 71.40 to read as follows:
§ 71.36 Medical examinations.
(a) The CDC may require that an individual arriving into the United States undergo a medical examination as part of a Federal order for quarantine, isolation, or conditional release.
(b) The CDC shall promptly arrange for the medical examination to be conducted when one is required under this section.
(c) As part of the medical examination, the CDC may require that an individual provide information and undergo such testing as may be reasonably necessary to diagnose or confirm the presence, absence, or extent of infection with a quarantinable communicable disease.
(d) Individuals reasonably believed to be infected based on the results of a medical examination may be isolated, or if such results are inconclusive or unavailable, individuals may be quarantined or conditionally released in accordance with this part.
§ 71.37 Requirements relating to issuance of a Federal order for quarantine, isolation, or conditional release.
(a) A Federal order authorizing quarantine, isolation, or conditional release shall be in writing, signed by a CDC authorizing official, and contain the following information:
(1) The identity of the individual or group subject to the order;
(2) The location of the quarantine or isolation or, in the case of conditional release, the entity to who and means by which the individual shall report for public health supervision;
(3) An explanation of the factual basis underlying the CDC’s reasonable belief that the individual is exposed to or infected with a quarantinable communicable disease;
(4) An explanation of the process for reassessment and medical review of the Federal order pursuant to this part; and
(5) An explanation of the criminal penalties for violating a Federal order of quarantine, isolation, or conditional release.
(b) A Federal order authorizing quarantine, isolation, or conditional release shall be promptly served on the individual, except that the Federal order may be published or posted in a conspicuous location if applicable to a group of individuals and individual service would be impracticable.
§ 71.38 Mandatory reassessment of a Federal order for quarantine, isolation, or conditional release (surveillance).
(a) The CDC shall reassess the need to continue the quarantine, isolation, or conditional release of an individual no later than 72 hours after the service of the Federal order.
(b) As part of the reassessment, the CDC shall review all records considered in issuing the Federal order, including travel records, records evidencing exposure or infection with a quarantinable communicable disease, as well as any relevant new information.
(c) As part of the reassessment, and where applicable, the CDC shall consider whether less restrictive alternatives would adequately serve to protect the public health.
(d) At the conclusion of the reassessment, the CDC shall promptly issue a written Federal order directing that the quarantine, isolation, or conditional release be continued, modified, or rescinded.
(e) In the event that the CDC directs that the quarantine, isolation, or conditional release be continued or modified, the written Federal order shall explain the process for requesting a medical review under this part.
(f) The CDC’s written Federal order shall be promptly served on the individual, except that the Federal order may be served by publication or by posting in a conspicuous location if applicable to a group of individuals and individual service would be impracticable.
§ 71.39 Medical review of a Federal order for quarantine, isolation, or conditional release.
(a) The CDC shall, as soon as practicable, arrange for a medical review upon a request by an individual under Federal quarantine, isolation, or conditional release.
(b) A request for a medical review may only occur after the CDC’s mandatory reassessment under § 71.38 and following the issuance of a Federal order continuing or modifying the quarantine, isolation, or conditional release.
(c) The medical review shall be for the purpose of ascertaining whether the CDC has a reasonable belief that the individual is infected with a quarantinable communicable disease.
(d) The CDC shall notify the individual in writing of the time and place of the medical review.
(e) The CDC shall designate a medical reviewer to review the medical or other evidence presented at the review, make medical or other findings of fact, and issue a recommendation concerning whether the Federal order for quarantine, isolation, or conditional release should be rescinded, continued, or modified.
(f) The individual subject to Federal quarantine, isolation, or conditional release may authorize a representative at his or her own expense to submit medical or other evidence and, in the medical reviewer’s discretion, be allowed to present a reasonable number of medical experts. The CDC shall appoint a medical representative at its own expense to assist the individual for purposes of the medical review upon a request and certification, under penalty of perjury, by that individual that he/she is indigent and cannot afford a medical representative.
(g) Prior to the convening of the review, the individual or his/her authorized representative shall be provided a reasonable opportunity to examine the available medical and other records involved in the medical review pertaining to that individual.
(h) The CDC shall take such measures that it determines to be reasonably necessary to allow an individual under Federal quarantine or isolation to communicate with an authorized representative in such a manner as to prevent the possible spread of the quarantinable communicable disease.
(i) The medical reviewer may order a medical examination of an individual when, in the medical reviewer’s professional judgment, such an examination would assist in assessing the individual’s medical condition.
(j) As part of the review, and where applicable, the medical reviewer shall consider and accept into the record evidence concerning whether less restrictive alternatives would adequately serve to protect public health.
(k) In the medical reviewer’s discretion, the review may be conducted through written submission, by telephone, or through any other means that the medical reviewer determines to be acceptable.
(l) At the conclusion of the review, the medical reviewer shall, based upon his or her review of the facts and other evidence made available during the medical review, issue a written report to the Director as to whether, in the medical reviewer’s professional judgment, the Federal quarantine, isolation, or conditional release should continue. The written report shall be served on the individual and the individual’s authorized representative.
(m) The Director shall, as soon as practicable, review the written report and any objections that may be submitted by the individual or the individual’s representative that contest the findings and recommendation contained in the medical reviewer’s written report. Upon conclusion of the review, the Director shall promptly issue a written Federal order directing that the quarantine, isolation, or conditional release be continued, modified, or rescinded. In the event that the Director continues or modifies the Federal quarantine, isolation, or conditional release, the Director’s written order shall include a statement that the individual may request that the CDC rescind the Federal quarantine, isolation, or conditional release, but based only on a showing of significant, new or changed facts or medical evidence that raise a genuine issue as to whether the individual should continue to be subject to Federal quarantine, isolation, or conditional release. The written Federal order shall be promptly served on the individual and the individual’s authorized representative, except that the Federal order may be served by publication or by posting in a conspicuous location if applicable to a group of individual’s and individual service would be impracticable.
(n) The Director’s written order shall not constitute final agency action until it has been served on the individual or the individual’s authorized representative, or alternatively, if applicable to a group of individuals and individual service would be impracticable, it is published or posted.
(o) The Director may order the consolidation of one or more medical reviews if the number of individuals or other factors makes the holding of individual medical reviews impracticable.
(p) The CDC may issue additional instructions as may be necessary or desirable governing the conduct of medical reviews.
§ 71.40 Agreements.
CDC may enter into an agreement with an individual, upon such terms as the CDC considers to be reasonably necessary, indicating that the individual consents to any of the public health measures authorized under this part, including quarantine, isolation, conditional release, medical examination, hospitalization, vaccination, and treatment; provided that the individual’s consent shall not be considered as a prerequisite to any exercise of any authority under this part.
15.Add § 71.63 to read as follows:
§ 71.63 Suspension of entry of animals, articles, or things from designated foreign countries and places into the United States.
(a) The CDC may suspend the entry into the United States of animals, articles, or things from designated foreign countries (including political subdivisions and regions thereof) or places whenever the Director determines that such an action is necessary to protect the public health and upon a finding that:
(1) There exists in a foreign country (including one or more political subdivisions and regions thereof) or place a communicable disease the introduction, transmission, or spread of which would threaten the public health of the United States; and
(2) The entry of imports from that country or place increases the risk that the communicable disease may be introduced, transmitted, or spread into the United States.
(b) The Director shall designate the foreign countries or places and the period of time or conditions under which the introduction of imports into the United States shall be suspended. HHS/CDC will coordinate in advance with other Federal agencies that have overlapping authority in the regulation of entry of animals, articles, or other things, as may be necessary to implement and enforce this provision.
Dated: July 12, 2016.
Sylvia M. Burwell,
Secretary.
[FR Doc. 2016-18103 Filed 8-12-16; 8:45 am]
BILLING CODE 4163-18-P
FOOTNOTESBack to Top
1. 42 U.S.C. 264 and 265 by their terms grant authority to the U.S. Surgeon General. The Reorganization Plan No. 3 of 1966 abolished the Office of the Surgeon General and transferred the Surgeon General’s functions to the Secretary of Health, Education, and Welfare (now Secretary of HHS). 31 FR 8855, 80 Stat. 1610 (Jun. 25, 1966). The Secretary of Health, Education, and Welfare was re-designated the Secretary of Health and Human Services by section 509(b) of Public Law 96-88, 93 Stat. 695 (codified at 20 U.S.C. 3508(b)). Although the Office of the Surgeon General was re-established in 1987, the Secretary of HHS has retained her authorities under 42 U.S.C. 264, 265.
2. The Executive Order defines severe acute respiratory syndromes as follows: “Severe acute respiratory syndromes, which are diseases that are associated with fever and signs and symptoms of pneumonia or other respiratory illness, are capable of being transmitted from person to person, and that either are causing, or have the potential to cause, a pandemic, or, upon infection, are highly likely to cause mortality or serious morbidity if not properly controlled. This subsection does not apply to influenza.”
3. The functions of the President under sections 362 and 364(a) of the Public Health Service Act (42 U.S.C. 265 and 267(a)) have been assigned to the HHS Secretary. See Exec. Order 13295 (Apr. 4, 2003), as amended by Exec. Order 13375 (Apr. 1, 2005) and Exec. Order 13674 (July 31, 2014).
4. “Glossary of Epidemiology Terms.” Centers for Disease Control and Prevention Resource Library, 2014. Web, accessed 15 July 2014.
5. “Ebola Hemorrhagic Fever: Ebolavirus Ecology.” CDC.gov, 2014. Web, accessed 8 July 2014.
6. Vogel, Gretchen. “Are Bats Spreading Ebola Across Sub-Saharan Africa?” Science, 2014. Vol. 344: p.140
7. Bagcchi, Sanjeet. “Ebola haemorrhagic fever in west Africa.” The Lancet, 2014. Vol. 14: p.375
8. Baize, Sylvain, et al. “Emergence of Zaire Ebola Virus Disease in Guinea—Preliminary Report.” The New England Journal of Medicine, 2014 (NEJM.ORG).
10. Case numbers obtained from the World Health Organization (http://apps.who.int/ebola/ebola-situation-reports).
12. Cases were exported to United States (2), United Kingdom, Nigeria, Mali (2), Senegal, Italy; further spread occurred in Nigeria, the United States and Mali.
13. See 79 FR 63313 (October 23, 2014).
14. Refer to the RIA for more details.
15. CDC. Measles Outbreak—California, December 2014-February 2015. Morb Mortal Wkly Rep. 2015; 64(06): 153-154. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6406a5.htm.
16. See Criteria for Requesting Federal Travel Restrictions for Public Health Purposes, Including for Viral Hemorrhagic Fevers, 80 FR 16,400 (Mar. 27, 2015).
17. See 19 CFR 122.49a for a list of the elements CBP requires for inbound commercial air travel.
18. Under APIS, address while in the United States (number and street, city, state, and zip code), except that this information is not required for U.S. citizens, lawful permanent residents, or persons who are in transit to a location outside the United States.
19. http://www.cdc.gov/vhf/ebola/about.html.
2. Smith I and Wange LF. Bats and their virome: An important source of emerging viruses capable of infecting humans Curr Opin Virol. 2013 (Feb;3(2):84-91.
3. Yang J, Zhang Y, Li J, et al. Serological evidence of ebolavirus infection in bats, China. Virol J. 2012 Oct. 13;9:236.
4. OLson SH, Reed P, Cameron KN, et al. Dead or alive: animal sampling during Ebola hemorrhagic fever outbreaks in humans. Emerg Health Threat J. 2012;5.
23. Leroy EM, Epelboin A, Mondonge V, et al. Human Ebola outbreak resulting from direct exposure to fruit bats in Luebo, Democratic Republic of Congo, 2007. Vector Borne Zoonotic Dis. 2009 Dec;9(6):723-8.
24. Leroy EM, Kumulungui B, Pourrut X, et al. Fruit bats as reservoirs of Ebola virus. Nature. 2005 Dec 1;438(7068):575-6.
25. The President. Presidential documents. Executive Order 12866 of September 30, 1993: Regulatory Planning and Review. Federal Register. Monday, October 4, 1993;58(190). http://www.archives.gov/Federal-register/executive-orders/pdf/12866.pdf. Accessed January 2016.
26. The President. Presidential documents. Executive Order 13563 of January 18, 2011: Improving Regulation and Regulatory Review. Federal Register. Friday, January 21, 2011; 76(14). http://www.gpo.gov/fdsys/pkg/FR-2011-01-21/pdf/2011-1385.pdf. Accessed January 2016.
27. U.S. Small Business Administration. Regulatory Flexibility Act. http://www.sba.gov/advocacy/823. Accessed January 2016.
28. Summary of the Unfunded Mandates Reform Act. 2 U.S.C. 1501 et seq. (1995). http://www2.epa.gov/laws-regulations/summary-unfunded-mandates-reform-act. Accessed January 2016.
29. Federal Register 62353 Vol. 68, No. 213 Tuesday, November 4, 2003. P. 62353-69.
30. Rassy D, Smith RD. The economic impact of H1N1 on Mexico’s tourist and pork sectors. Health Econ. 2013;22(7):824-34. doi: 10.1002/hec.2862. PubMed PMID: 23744805.
31. Keogh-Brown MR, Smith RD. The economic impact of SARS: How does the reality match the predictions? Health Policy. 2008;88(1):110-20.
32. Gastañaduy, P.A., S.B. Redd, A.P. Fiebelkorn, J.S. Rota, P.A. Rota, W.J. Bellini, J.F. Seward and G.S. Wallace (2014). “Measles — United States, January 1-May 23, 2014.” MMWR 63(22): 496-499.
33. Nelson, K., Marienau, K.J., Schembri, C. and Redd, S. (2013). “Measles transmission during air travel, United States.” Travel Medicine and Infectious Disease (2013) 11, 81e89 11: 81-89.
34. Nelson, K., Marienau, K.J., Schembri, C. and Redd, S. (2013). “Measles transmission during air travel, United States.” Travel Medicine and Infectious Disease (2013) 11, 81e89 11: 81-89.
35. Ortega-Sanchez, I.R., M. Vijayaraghavan, A.E. Barskey and G.S. Wallace (2012). “The economic burden of sixteen measles outbreaks on United States public health departments in 2011.” Vaccine 32(11).
36. Jennifer Zipprich, Kathleen Winter, Jill Hacker, Dongxiang Xia, James Watt, Kathleen Harriman. (2015) Measles Outbreak — California, December 2014-February 2015. MMWR/February 20, 2015/Vol. 64/No. 6: 153-154.
37. Ortega-Sanchez, I.R., M. Vijayaraghavan, A.E. Barskey and G.S. Wallace (2012). “The economic burden of sixteen measles outbreaks on United States public health departments in 2011.” Vaccine 32(11).
40. U.S. Department of Transportation, Federal Aviation Administration (January 2015) The Economic Impact of Civil Aviation on the U.S. Economy: Economic Impact of Civil Aviation by State. http://www.faa.gov/air_traffic/publications/media/2015-economic-impact-report.pdf (Accessed 5/2/2016).
41. Bureau of Transportation Statistics T-100 Market data. http://www.transtats.bts.gov/Data_Elements.aspx?Data=1 (Accessed 5/2/2016).
42. U.S. Department of Transportation Maritime Administration (March 2012) North American Cruise Statistical Snapshot, 2011 http://www.marad.dot.gov/wp-content/uploads/pdf/North_American_Cruise_Statistics_Quarterly_Snapshot.pdf (Accessed 5/2/2016).
43. According to the U.S. Department of Homeland Security, 54,236 passengers and crew arrive via vessel each day, which correspond to approximately 18 million per year. https://www.transportation.gov/policy/aviation-policy/us-international-air-passenger-and-freight-statistics-reportAccessed on 5/2/2106.
45. Personal communication between Dr. Brian Maskery and DOT/FAA.
47. Margaret S. Coleman, unpublished data.
48. Coleman, M.S., Marienau, K.J., Marano, N., Marks, S.M., Cetron, M.S. (2014). “Economics of United States tuberculosis airline contact investigation policies: a return on investment analysis.” TMAID 12(1):63-71.
49. Personal communication from states to Dr. Margaret S. Coleman 2010.
50. Discussion between Dr. Brian Maskery, Dr. Margaret S. Coleman and State and County Health Department contacts 11/21/2014.
51. Nelson, K., Marienau, K. J., Schembri, C. and Redd, S. (2013). “Measles transmission during air travel, United States.” Travel Medicine and Infectious Disease (2013) 11, 81e89 11: 81-89.
52. Nelson, K., Marienau, K. J., Schembri, C. and Redd, S. (2013). “Measles transmission during air travel, United States.” Travel Medicine and Infectious Disease (2013) 11, 81e89 11: 81-89.
53. Nelson, K., Marienau, K. J., Schembri, C. and Redd, S. (2013). “Measles transmission during air travel, United States.” Travel Medicine and Infectious Disease (2013) 11, 81e89 11: 81-89.
54. Smith P, Marcuse E, Seward J, Zhao Z, WA O. Children and Adolescents Unvaccinated Against Measles: Geographic Clustering, Parents’ Beliefs, and Missed Opportunities. Public Health Rep. 2015;5:485-504.
55. Ko G, Thompson KM, Nardell EA. Estimation of tuberculosis risk on a commercial airliner. Risk Anal 2004;24:379e88.
56. Marienau KJ, Cramer EH, Coleman MS, Marano N, Cetron MS. Flight related tuberculosis contact investigations in the United States: Comparative risk and economic analysis of alternate protocols. Travel Med Infect Dis. 2014;12(1):54-62.
57. Marienau KJ, Burgess GW, Cramer E, et al. Tuberculosis investigations associated with air travel: US Centers for Disease Control and Prevention, January 2007-June 2008. Travel Med Infect Dis 2010;8:104e12.
58. Marienau KJ, Burgess GW, Cramer E, et al. Tuberculosis investigations associated with air travel: US Centers for Disease Control and Prevention, January 2007-June 2008. Travel Med Infect Dis 2010;8:104e12.
59. Coleman M, Marienau K, Marano N, Marks S, Cetron M, Dis TMI. Economics of United States Tuberculosis Airline Contact Investigation Policies. Travel Medicine and Infectious Disease. 2014;12:63-71.
60. Marienau KJ, Burgess GW, Cramer E, et al. Tuberculosis investigations associated with air travel: US Centers for Disease Control and Prevention, January 2007-June 2008. Travel Med Infect Dis 2010;8:104e12.
61. Mangili A, Gendreau MA. Transmission of infectious diseases during commercial air travel. Lancet. 2005;365:989-96.
62. Anderson RM. The concept of herd immunity and the design of community-based immunization programmes. Vaccine. 1992;10(13):928-35.
63. Chapter 14. Meningococcal Disease, The Pink Book, CDC http://www.cdc.gov/vaccines/pubs/pinkbook/mening.html Accessed 5/2/2016.
64. Marienau KJ, Burgess GW, Cramer E, et al. Tuberculosis investigations associated with air travel: US Centers for Disease Control and Prevention, January 2007-June 2008. Travel Med Infect Dis 2010;8:104e12.
65.
66. Nelson K, Marienau K, Schembri C, Redd S. Measles transmission during air travel, United States. Travel Medicine and Infectious Disease (2013) 11, 81e89. 2013;11:81-9.
67. P Kutty, J Rota, W Bellini, SB Redd, A Barskey, G Wallace. (2014) Manual for the Surveillance of Vaccine-Preventable Diseases: Chapter 7 Measles. http://www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html. Accessed 5/8/2016.
68. CDC (2015) Epidemiology and Prevention of Vaccine-Preventable Diseases: Measles. http://www.cdc.gov/vaccines/pubs/pinkbook/meas.html. Accessed 5/8/2016.
69. Nelson, K., Marienau, K. J., Schembri, C. and Redd, S. (2013). “Measles transmission during air travel, United States.” Travel Medicine and Infectious Disease (2013) 11, 81e89 11: 81-89.
70. http://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/archive.html Accessed 5/2/2016.
71. InGauge Healthcare Solutions. 2015 Physicians’ Fee & Coding Guide. Atlanta GA2013.
72. Ortega-Sanchez IR, Vijayaraghavan M, Barskey AE, Wallace GS. The economic burden of sixteen measles outbreaks on United States public health departments in 2011. Vaccine. 2012;32(11).
73. Ortega-Sanchez IR, Vijayaraghavan M, Barskey AE, Wallace GS. The economic burden of sixteen measles outbreaks on United States public health departments in 2011. Vaccine. 2012;32(11).
74. Zhou F, Shefer A, Wenger J, Messonnier M, Wang LY, Lopez A, et al. Economic Evaluation of the Routine Childhood Immunization Program in the United States, 2009. Pediatrics. 2014;133:577-85.
75. Mason WH, Ross LA, Lanson J, Wright HT. Epidemic measles in the postvaccine era: evaluation of epidemiology, clinical presentation, and complications during an urban outbreak. Pediatr Infect Dis J. 1993;12:42-8.
76. Centers for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases, 13th Edition- Measles April 2015 http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/meas.pdfAccessed 6/13/2016.
77. Coleman M, Marienau K, Marano N, Marks S, Cetron M, Dis TMI. Economics of United States Tuberculosis Airline Contact Investigation Policies. Travel Medicine and Infectious Disease. 2014;12:63-71.
78. Coleman M, Marienau K, Marano N, Marks S, Cetron M, Dis TMI. Economics of United States Tuberculosis Airline Contact Investigation Policies. Travel Medicine and Infectious Disease. 2014;12:63-71.
79. Nelson K, Marienau K, Schembri C, Redd S. Measles transmission during air travel, United States, December 1, 2008-December 31, 2011. Travel Med Infect Dis. 2013;11(2):81-9.
80. Nelson KR, Marienau KJ, Barskey AE, Schembri C. No evidence of mumps transmission during air travel, United States, November 1, 2006—October 31, 2010. Travel Medicine and Infectious Disease. 2012;10:165-71.
81. Marienau KJ, Cramer EH, Coleman MS, Marano N, Cetron MS. Flight related tuberculosis contact investigations in the United States: comparative risk and economic analysis of alternate protocols. Travel Med Infect Dis. 2014;12(1):54-62.
82. SteelFisher GK, Blendon RJ, Lasala-Blanco N. Ebola in the United States—Public Reactions and Implications. N Eng J Med. 2015;373:789-91.
83. Chevalier MS, Chung W, Smith J, et al. Ebola virus disease cluster in the United States—Dallas County, Texas, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1087-8.
84. McCarty CL, Basler C, Karwowski M, et al. Response to importation of a case of Ebola virus disease—Ohio, October 2014. MMWR Morb Mortal Wkly Rep 2014;63:1089-91.
85. Regan JJ, Jungerman R, Montiel SH, et al. Public health response to commercial airline travel of a person with Ebola virus infection—United States, 2014. MMWR Morb Mortal Wkly Rep 2015;64:63-6.
86. Yacisin K, Balter S, Fine A, et al. Ebola virus disease in a humanitarian aid worker—New York City, October 2014. MMWR Morb Mortal Wkly Rep 2015;64:321-3.
87. McAuliff M. Lawmakers ignore experts, push for Ebola travel ban. The Huffington Post. October 16, 2014. http://www.huffingtonpost.com/2014/10/16/congress-ebola_n_5997214.html9. Nuzzo JB, Cicero AJ, Waldhorn R, Inglesby TV. Travel bans will increase the damage wrought by Ebola. Biosecur Bioterror 2014;12:306-9. http://dx.doi.org/10.1089/bsp.2014.1030
88. Nuzzo JB, Cicero AJ, Waldhorn R, Inglesby TV. Travel bans will increase the damage wrought by Ebola. Biosecur Bioterror 2014;12:306-9. http://dx.doi.org/10.1089/bsp.2014.1030
89. Poletto C, Gomes MF, Pastore y Piontti A, et al. Assessing the impact of travel restrictions on international spread of the 2014 West African Ebola epidemic. Euro Surveill 2014;19:pii 20936. http://dx.doi.org/10.2807/1560-7917.ES2014.19.42.20936
90. Frieden T. CDC Chief: Why I don’t support a travel ban to combat Ebola outbreak (2014). http://www.foxnews.com/opinion/2014/10/09/cdc-chief-why-dont-support-travel-ban-to-combat-ebola-outbreak.html Accessed 6/9/2015.
91. Anderson M. Ebola: airlines cancel more flights to affected countries. The Guardian. August 22, 2014. http://www.theguardian.com/society/2014/aug/22/ebola-airlines-cancel-flights-guinea-liberia-sierra-leone. Accessed 6/9/2016.
92. Balen B. Ebola supplies sit as airlines cancel flights to countries with infection. The Guardian. September 8, 2014. http://guardianlv.com/2014/09/ebola-supplies-sit-as-airlines-cancel-flights-to-countries-with-infection/. Accessed 6/9/3026.
93. Anderson M. Ebola: airlines cancel more flights to affected countries. The Guardian. August 22, 2014. http://www.theguardian.com/society/2014/aug/22/ebola-airlines-cancel-flights-guinea-liberia-sierra-leone. Accessed 6/9/2016.
94. Chevalier MS, Chung W, Smith J, et al. Ebola virus disease cluster in the United States—Dallas County, Texas, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1087-8.
95. Yacisin K, Balter S, Fine A, et al. Ebola virus disease in a humanitarian aid worker—New York City, October 2014. MMWR Morb Mortal Wkly Rep 2015;64:321-3.
96. Gulland A. Second Ebola patient is treated in UK. BMJ 2014;349:g7861. http://dx.doi.org/10.1136/bmj.g7861 PubMed.
97. World Health Organization. Ebola virus disease—Italy. Disease Outbreak News, May 13, 2015. http://www.who.int/csr/don/13-may-2015-ebola/en/.
98. Brown CM, Aranas AE, Benenson GA, et al. Airport exit and entry screening for Ebola—August-November 10, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1163-7.
99. CDC. Notes on the interim U.S. guidance for monitoring and movement of persons with potential Ebola virus exposure. February 19, 2016. http://www.cdc.gov/vhf/ebola/exposure/monitoring-and-movement-of-persons-with-exposure.html.
100. Chevalier MS, Chung W, Smith J, et al. Ebola virus disease cluster in the United States—Dallas County, Texas, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1087-8.
101. Regan JJ, Jungerman R, Montiel SH, et al. Public health response to commercial airline travel of a person with Ebola virus infection—United States, 2014. MMWR Morb Mortal Wkly Rep 2015;64:63-6.
102. Bever L. Chain reaction: concern about Ebola nurse’s flight prompts school closings in two states. The Washington Post. October 16, 2014. https://www.washingtonpost.com/news/morning-mix/wp/2014/10/16/after-concern-about-ebola-patients-flight-schools-close-in-two-cities/.
103. Mejia P. Planes, automobiles and cruise ships: vehicles for Ebola panic. Newsweek. October 17, 2014. http://www.newsweek.com/planes-automobiles-and-cruise-ships-vehicles-ebola-panic-278206
104. Yacisin K, Balter S, Fine A, et al. Ebola virus disease in a humanitarian aid worker—New York City, October 2014. MMWR Morb Mortal Wkly Rep 2015;64:321-3.
105. Spencer C. Having and fighting Ebola—public health lessons from a clinician turned patient. N Engl J Med 2015;372:1089-91. http://dx.doi.org/10.1056/NEJMp1501355.
106. Chevalier MS, Chung W, Smith J, et al. Ebola virus disease cluster in the United States—Dallas County, Texas, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1087-8.
107. Yacisin K, Balter S, Fine A, et al. Ebola virus disease in a humanitarian aid worker—New York City, October 2014. MMWR Morb Mortal Wkly Rep 2015;64:321-3.
108. Forrester JD, Hunter JC, Pillai SK, et al. Cluster of Ebola cases among Liberian and U.S. health care workers in an Ebola treatment unit and adjacent hospital—Liberia, 2014. MMWR Morb Mortal Wkly Rep 2014;63:925-9. PubMed.
109. Matanock A, Arwady MA, Ayscue P, et al. Ebola virus disease cases among health care workers not working in Ebola treatment units—Liberia, June-August, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1077-81.
110. McAuliff M. Lawmakers ignore experts, push for Ebola travel ban. The Huffington Post. October 16, 2014. http://www.huffingtonpost.com/2014/10/16/congress-ebola_n_5997214.html.
111. Infectious Diseases Society of America. IDSA statement on involuntary quarantine of healthcare workers returning from Ebola-affected countries. http://www.idsociety.org/2014_ebola_quarantine/.
112. Devaney T. Fauci calls Ebola quarantines “draconian.” The Hill. October 26, 2014. http://thehill.com/policy/healthcare/221890-top-nih-officials-calls-quarantines-draconian.
113. American Civil Liberties Union; Yale Global Health Justice Partnership. Fear, politics, and Ebola: how quarantines hurt the fight against Ebola and violate the Constitution. December 2015. https://www.aclu.org/sites/default/files/field_document/aclu-ebolareport.pdf.
114. Sun L.H. Cost to treat Ebola in the U.S.: $1.16 million for 2 patients. Washington Post November 18, 2014 https://www.washingtonpost.com/news/post-nation/wp/2014/11/18/cost-to-treat-ebola-in-the-u-s-1-16-million-for-2-patients/?utm_term=.283370dc6c47. Accessed6/10/2016.
115. Bureau of Labor Statistics May 2015 National Occupational Employment and Wage Estimates United States. http://www.bls.gov/oes/current/oes_nat.htm. Accessed 6/12/2016.
116. Sunshine G, Pepin D, Cetron M, Penn M. State and Territorial Ebola Screening, Monitoring, and Movement Policy Statements — United States, August 31, 2015. Morbidity and Mortality Weekly Report (MMWR). 2015;64(40):1145-6.
117. Weber DJ, William A. Rutala, William A. Fischer, Hajime Kanamori, Sickbert-Bennett EE. Emerging infectious diseases: Focus on infection control issues for novel coronaviruses (Severe Acute Respiratory Syndrome-CoV and Middle East Respiratory Syndrome-CoV), hemorrhagic fever viruses (Lassa and Ebola), and highly pathogenic avian influenza viruses, A(H5N1) and A(H7N9) American Journal of Infection Control. 2016;44(5):e91-e100.
118. Chevalier MS, Chung W, Smith J, et al. Ebola virus disease cluster in the United States—Dallas County, Texas, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1087-8.
119. McCarty CL, Basler C, Karwowski M, et al. Response to importation of a case of Ebola virus disease—Ohio, October 2014. MMWR Morb Mortal Wkly Rep 2014;63:1089-91.
120. Chevalier MS, Chung W, Smith J, et al. Ebola virus disease cluster in the United States—Dallas County, Texas, 2014. MMWR Morb Mortal Wkly Rep 2014;63:1087-8
121. Chung WM, Smith JC, Weil LM, Hughes SM, Joyner SN, Hall EM, et al. Active Tracing and Monitoring of Contacts Associated With the First Cluster of Ebola in the United States. Ann Intern Med. 2015;163:164-73.
122. Chung WM, Smith JC, Weil LM, Hughes SM, Joyner SN, Hall EM, et al. Active Tracing and Monitoring of Contacts Associated With the First Cluster of Ebola in the United States. Ann Intern Med. 2015;163:164-73.
123. Regan JJ, Jungerman R, Montiel SH, et al. Public health response to commercial airline travel of a person with Ebola virus infection—United States, 2014. MMWR Morb Mortal Wkly Rep 2015;64:63-6.
124. Bever L. Chain reaction: concern about Ebola nurse’s flight prompts school closings in two states. The Washington Post. October 16, 2014. https://www.washingtonpost.com/news/morning-mix/wp/2014/10/16/after-concern-about-ebola-patients-flight-schools-close-in-two-cities/.
125. Yacisin K, Balter S, Fine A, et al. Ebola virus disease in a humanitarian aid worker—New York City, October 2014. MMWR Morb Mortal Wkly Rep 2015;64:321-3.
126. Smith CL, Hughes SM, Karwowski MP, Chevalier MS, Hall E, Joyner SN, et al. Addressing Needs of Contacts of Ebola Patients During an Investigation of an Ebola Cluster in the United States—Dallas, Texas, 2014. Morbidity and Mortality Weekly Report (MMWR). 2015;64(5).
127. West, M.G. The high cost of quarantine The Wall Street Journal. October 29, 2014. http://www.wsj.com/articles/the-high-cost-of-quarantine-and-who-pays-for-it-1414546114. Accessed June 13, 2016.
129. Sun L.H. Cost to treat Ebola in the U.S.: $1.16 million for 2 patients. Washington Post November 18, 2014 https://www.washingtonpost.com/news/post-nation/wp/2014/11/18/cost-to-treat-ebola-in-the-u-s-1-16-million-for-2-patients/?utm_term=.283370dc6c47. Accessed 6/10/2016.
130. Worstall T. The Free Market Won’t Produce An Ebola Cure; So Should Government Instead? Forbes: August 8, 2014. http://www.forbes.com/sites/timworstall/2014/08/08/the-free-market-wont-produce-an-ebola-cure-so-should-government-instead/#f8f45d46cac5. Accessed June 13, 2016.
131. LaMantia, J. Hospitals bleed money as they fight Ebola. Crain’s New York Business. November 10, 2014. http://www.crainsnewyork.com/article/20141110/HEALTH_CARE/141119994/hospitals-bleed-money-as-they-fight-ebola. Accessed June 14, 2016.
132. SteelFisher GK, Blendon RJ, Lasala-Blanco N. Ebola in the United States—Public Reactions and Implications. N Eng J Med. 2015;373:789-91.
133. SteelFisher GK, Blendon RJ, Lasala-Blanco N. Ebola in the United States — Public Reactions and Implications. N Eng J Med. 2015;373:789-91.
134. Keogh-Brown M.R. and Smith R.D., The economic impact of SARS: How does the reality match the predictions? Health Policy. 2008; 88: 110-120.
135. Keogh-Brown M.R. and Smith R.D., The economic impact of SARS: How does the reality match the predictions? Health Policy. 2008; 88: 110-120.
136. Beutels P., Jia N, Zhou Q., et al., The economic impact of SARS in Beijing, China. Tropical Medicine and International Health, 2009, 12 Suppl 1: 85-91.
137. Korea Centers for Disease Control and Prevention. Middle East Respiratory Syndrome Coronavirus Outbreak in the Republic of Korea, 2015. Osong Public Health Research Perspective. 2015;6(4):269-78.
138. Marks S.M., Flood J., Seaworth, B., et al. Treatment practices, outcomes, and costs of multidrug-resistant and extensively drug-resistant tuberculosis, United States, 2005-2007. Emerging Infectious Disease. 2014; 20(5):812-820.
139. Korea Centers for Disease Control and Prevention. Middle East Respiratory Syndrome Coronavirus Outbreak in the Republic of Korea, 2015. Osong Public Health Research Perspective. 2015;6(4):269-78.
140. Bureau of Labor Statistics (http://www.bls.gov/oes/current/oes_nat.htm.
141. Cho K.Y., Yoo J.S. Forecasting Economic loss associated with MERS outbreak in South Korea, 2015. KERI Insight. 15-20.
142. Cauchemez S., Van Kerkhove M.D., Archer B.N. et al. School closures during the 2009 influenza pandemic: national and local experiences. BMC Infectious Disease. 2014; 14: 207.
143. Cauchemez S., Van Kerkhove M.D., Archer B.N. et al. School closures during the 2009 influenza pandemic: national and local experiences. BMC Infectious Disease. 2014; 14: 207.
144. Borse H.R., Behravesh C.B., Dumanovsky T. et al., Closing schools in response to the 2009 pandemic influenza A H1N1 virus in New York City: Economic impact on households. Clinical Infectious Disease: 2011; 52 (Supple 1) S168-S172.
145. Trends of foreign travelers, South Korean international travelers, tourism income, and tourism expenditure in December 2015, Korea Tourism Organization.
146. Trends of foreign travelers, South Korean international travelers, tourism income, and tourism expenditure in December 2015, Korea Tourism Organization.
147. Cho, K., Yoo, J., Forecasted economic losses due to MERS outbreak in South Korea, KERI Insight.
148. U.S. Central Intelligence Agency. The World Factbook. United States Economy. https://www.cia.gov/library/publications/the-world-factbook/geos/us.html. Accessed June 13, 2016.
149. Bogoch II, Creatore MI, Cetron MS, Brownstein JS, Pesik N, Miniota J, et al. Assessment of the potential for international dissemination of Ebola virus via commercial air travel during the 2014 west African outbreak. Lancet. 2015;385:29-35.
150. McAuliff M. Lawmakers ignore experts, push for Ebola travel ban. The Huffington Post. October 16, 2014. http://www.huffingtonpost.com/2014/10/16/congress-ebola_n_5997214.html.
151. Olliaro P, Lasry E, Tiffany A. Out of (West) Africa—Who Lost in the End? Am J Trop Med Hyg 2015 Feb 4; 92(2): 242-243. 2015;92(2):242-3.
152. Poletto C, Gomes M, Pastore y Piontti A, Rossi L, Bioglio L, Chao D, et al. Assessing the impact of travel restrictions on international spread of the 2014 West African Ebola epidemic. Euro Surveill. 2014;19(42):pii: 20936.
153. https://ustr.gov/countries-regions/africa/west-africa/liberia; https://ustr.gov/countries-regions/africa/west-africa/guinea; https://ustr.gov/countries-regions/africa/west-africa/sierra-leone Accessed June 13, 2016.
154. https://ustr.gov/countries-regions/africa/west-africa/liberia; https://ustr.gov/countries-regions/africa/west-africa/guinea; https://ustr.gov/countries-regions/africa/west-africa/sierra-leone Accessed June 13, 2016.
155. Marks SM, Flood J, Seaworth B, Hirsch-Moverman Y, Armstrong L, Mase S, et al. Treatment Practices, Outcomes, and Costs of Multidrug-Resistant and Extensively Drug-Resistant Tuberculosis, United States, 2005-2007. Emerging Infectious Diseases. 2014;20(5):812-20.
156. Marks S.M., Flood J., Seaworth, B., et al. Treatment practices, outcomes, and costs of multidrug-resistant and extensively drug-resistant tuberculosis, United States, 2005-2007. Emerging Infectious Disease. 2014; 20(5):812-820.
157. Sun L.H. Cost to treat Ebola in the U.S.: $1.16 million for 2 patients. Washington Post November 18, 2014.
158. Worstall T. The Free Market Won’t Produce An Ebola Cure; So Should Government Instead? Forbes: August 8, 2014. http://www.forbes.com/sites/timworstall/2014/08/08/the-free-market-wont-produce-an-ebola-cure-so-should-government-instead/#f8f45d46cac5 Accessed June 13, 2016.
159. Sun L.H. Cost to treat Ebola in the U.S.: $1.16 million for 2 patients. Washington Post November 18, 2014 https://www.washingtonpost.com/news/post-nation/wp/2014/11/18/cost-to-treat-ebola-in-the-u-s-1-16-million-for-2-patients/?utm_term=.283370dc6c47. Accessed6/10/2016.
160. http://www.unicef.org/supply/files/MMR.pdf. Accessed 6/15/2016.
161. http://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/2015/2015-07-01.html#modalIdString_CDCTable_0. Accessed 6/15/2016.
162. Coleman M, Garbat-Welch L, Burke H, Weinberg M, Humbaugh K, Tindall A, et al. Direct costs of a single case of refugee-imported measles in Kentucky. Vaccine. 2012;30(2):317-21.
163. Federal Register 62353 Vol. 68, No. 213 Tuesday, November 4, 2003. P. 62353-69.
164. Federal Register 62353 Vol. 68, No. 213 Tuesday, November 4, 2003. P. 62353-69.
165. Khodakevich, L., Jezek, Z. and Messinger, D., “Monkeypox Virus: Ecology and Public Health Significance,” Bulletin of the World Health Organization, 66: 747-752, 1988. This reference identifies several species of squirrels as playing a major role as a reservoir for the monkeypox virus and Federal Register 62353 Vol. 68, No. 213 Tuesday, November 4, 2003. P. 62353-69.
166. Federal Register 62353 Vol. 68, No. 213 Tuesday, November 4, 2003. P. 62353-69.
167. https://www.ndhan.gov/data/health/CDC%20Advisory%2000183.pdf. Accessed on 5/2/2016.
168. Lankau E.W., Sinclair J.R. Schroeder B.A., Galland G.G., Marano N. Public health implications of changing rodent importation patterns—United States, 1999-2013, Transboundary and Emerging Diseases. 2015.
169. Schroeder, B., J. McQuiston, R. Marquis, G. Galland, and N. Marano, 2008: Anticipating the next monkeypox: Trends in rodent importation, 1999-2006. International Conference on Emerging Infectious Diseases, Atlanta GA (abstract, 2008).
170. Lankau E.W., Sinclair J.R., Schroeder B.A., Galland G.G., Marano N. Public health implications of changing rodent importation patterns—United States, 1999-2013, Transboundary and Emerging Diseases. 2015.
171. Lankau E.W., Sinclair J.R., Schroeder B.A., Galland G.G., Marano N. Public health implications of changing rodent importation patterns—United States, 1999-2013, Transboundary and Emerging Diseases. 2015.
172. Lankau E.W., Sinclair J.R., Schroeder B.A., Galland G.G., Marano N. Public health implications of changing rodent importation patterns—United States, 1999-2013, Transboundary and Emerging Diseases. 2015.
173. Lankau E.W., Sinclair J.R. Schroeder B.A., Galland G.G., Marano N. Public health implications of changing rodent importation patterns—United States, 1999-2013, Transboundary and Emerging Diseases. 2015.
174. Centers for Disease Control and Prevention (CDC). Update: Multistate outbreak of Monkeypox—Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. Morb Mort Weekly Rep, . 2003;52:642-6.
175. Centers for Disease Control and Prevention (CDC). Update: Multistate outbreak of Monkeypox—Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. Morb Mort Weekly Rep, . 2003;52:642-6.
176. Federal Register 62353 Vol. 68, No. 213 Tuesday, November 4, 2003. P. 62353-69.
177. Sejvar JJ, Chowdary Y, Schomogyi M, Stevens J, Patel J, Karem K, et al. Human Monkeypox Infection: A Family Cluster in the Midwestern United States. Journal of Infectious Diseases. 2004;190:1833-40.
178. Centers for Disease Control and Prevention (CDC). Update: Multistate outbreak of Monkeypox—Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. Morb Mort Weekly Rep 2003;52:642.
179. Centers for Disease Control and Prevention (CDC). Update: Multistate outbreak of Monkeypox—Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. Morb Mort Weekly Rep, . 2003;52:642-6.; Federal Register 62353 Vol. 68, No. 213 Tuesday, November 4, 2003. P. 62353-69.
180. State of Colorado, Wildlife Commission, “Emergency Regulation,” dated July 10, 2003.
181. State of Illinois, “Executive Order in Response to Orthopox Outbreak,” dated June 7, 2003.
182. State of Indiana, Board of Animal Health, Emergency Rule, dated June 9, 2003.
183. State of Michigan, Department of Community Health, “Order Finding Imminent Danger to the Public Health and Requiring Corrective Action,” dated June 13, 2003, and later amended on June 27, 2003.
184. State of North Dakota, State Board of Animal Health, “In the matter of: Monkeypox in Prairie Dogs and Gambian Giant pouched Rats,” Order No. 2003-04, dated June 11, 2003.
185. State of Wisconsin, Department of Agriculture, Trade, and Consumer Protection, “Emergency Rule,” dated June 9, 2003.
186. http://www.cdc.gov/poxvirus/monkeypox/outbreak.html. Accessed 5/2/2016.
187. http://www.bls.gov/oes/current/oes_nat.htm. Accessed 5/2/2016.
188. Federal Register 62353 Vol. 68, No. 213 Tuesday, November 4, 2003. P. 62353-69.
189. Ligon BL. Monkeypox: A review of the history and emergence in the Western hemisphere. Seminars in Pediatric Infectious Diseases. 2004; 15:280-7.
190. Kroeger T. Economic Impacts of Live Wild animal Imports in the United States. Defenders of Wildlife; 2004.
191. Healthcare Costs Institute. Healthcare Costs and Utilization Report. Washington DC: Health Care Costs Institute; 2011.
192. Healthcare Costs Institute. Healthcare Costs and Utilization Report. Washington DC: Health Care Costs Institute; 2011.
193. Reed KD, Melski JW, Graham MB, Regnery RL, Sotir MJ, Wegner MV, et al. The detection of monkeypox in humans in the western hemisphere. N Engl J Med 2004; 350:342-50.
194. http://www.bls.gov/oes/current/oes_nat.htm. Accessed 5/2/2016.
195. Healthcare Costs Institute. Healthcare Costs and Utilization Report. Washington DC: Health Care Costs Institute; 2011.
196. Centers for Disease Control and Prevention (CDC). Update: Multistate outbreak of Monkeypox—Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. Morb Mort Weekly Rep,. 2003;52:642—6.
197. Healthcare Costs Institute. Healthcare Costs and Utilization Report. Washington DC: Health Care Costs Institute; 2011.
198. Centers for Disease Control and Prevention (CDC). Update: Multistate outbreak of Monkeypox—Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003. Morb Mort Weekly Rep. 2003;52:642-6.






















































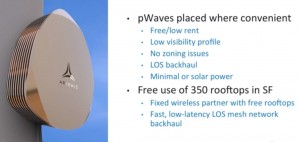


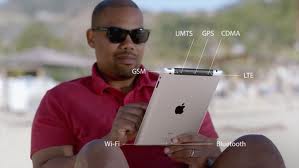







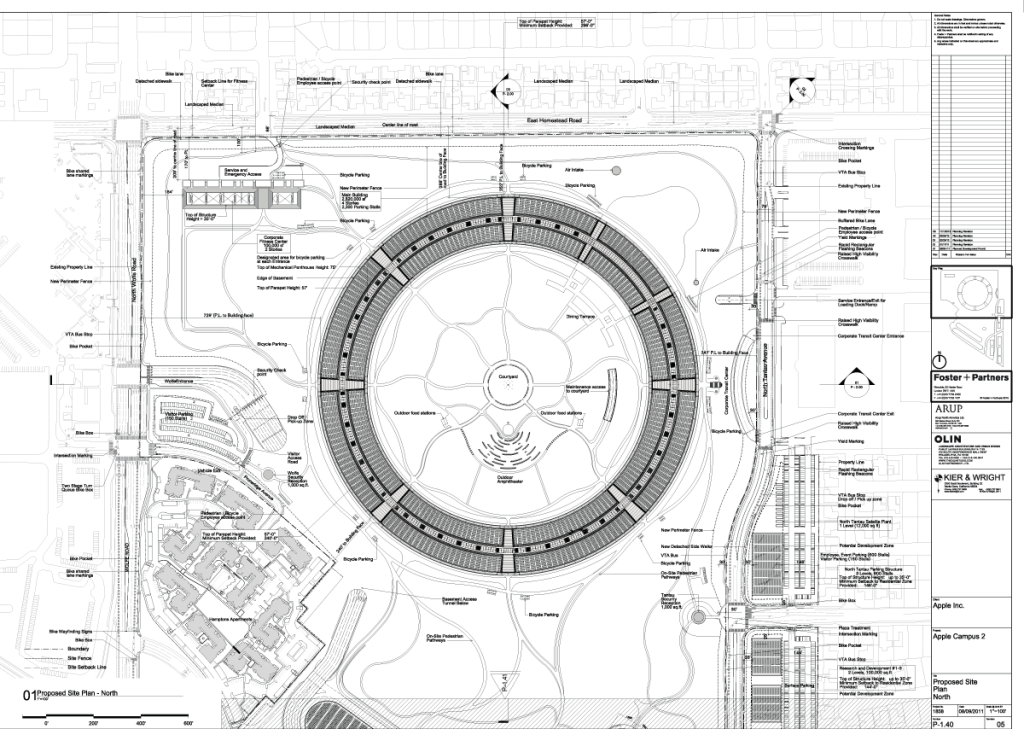
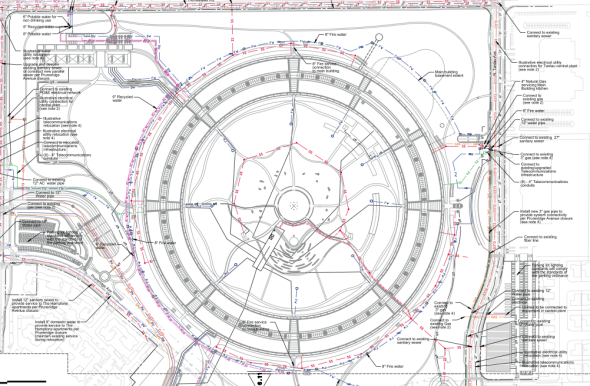
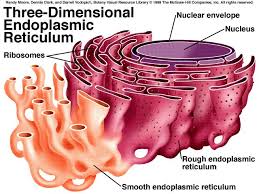
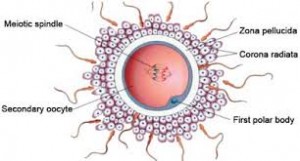
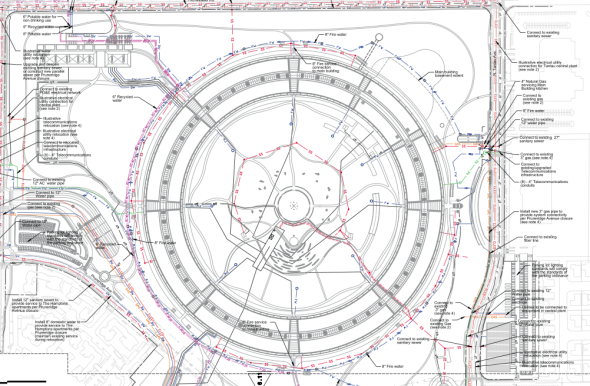




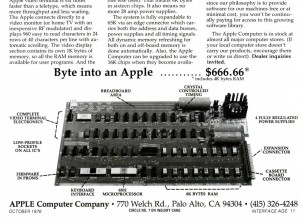

Recent Comments